Biologic Agents in Lymphocytic Scarring Alopecia
The field of dermatology has changed dramatically with the introduction of a variety of monoclonal antibodies, fusion proteins and growth factors to the list of treatment options. These agents are used to treat a wide range of disorders including psoriasis, hidradenitis suppurativa, atopic dermatitis, pyoderma gangrenosum, and various blistering diseases. This is by no means the full list.
The use of these agents in lymphocytic scarring alopecias like lichen planopilaris has been studied to a very limited degree. However their benefits are not entirely clear and many agents may actually worsen the disease. Here, we very briefly review some of the existing literature about the use of various biologic agents in treating LPP, including the monoclonal antibodies, fusion proteins and growth factors.
CATEGORY 1: Monoclonal Antibodies
Monoclonal antibodies are antibodies that target specific cell-surface receptors. These antibodies may be chimeric, humanized or human depending on how much murine and human proteins they contain.
a) Anti-TNF Antibodies: Adalimumab, Infliximab, Certolizumab, Golimumab
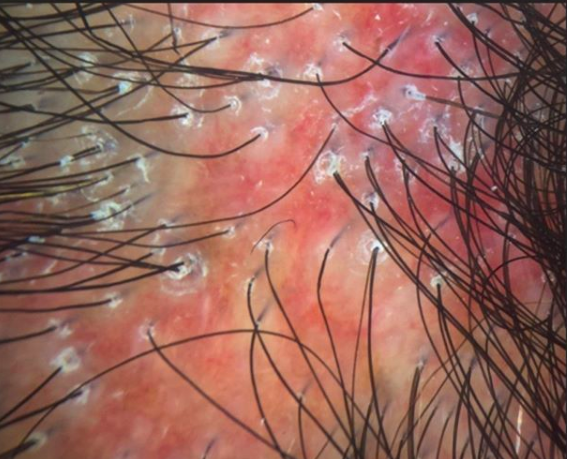
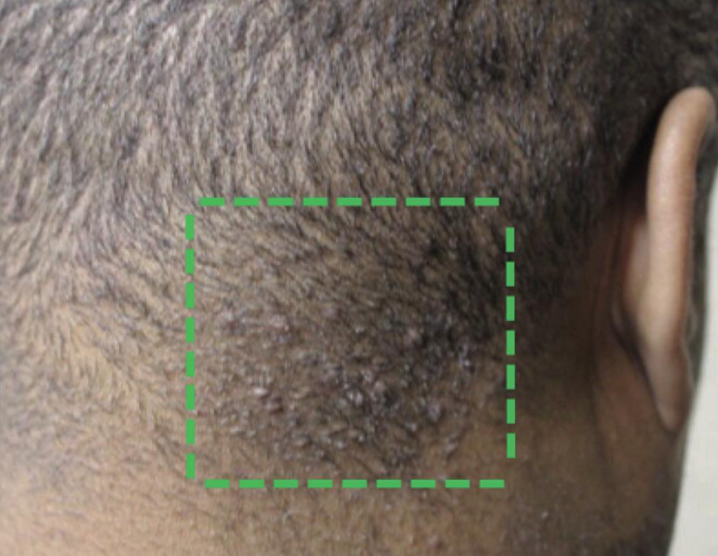
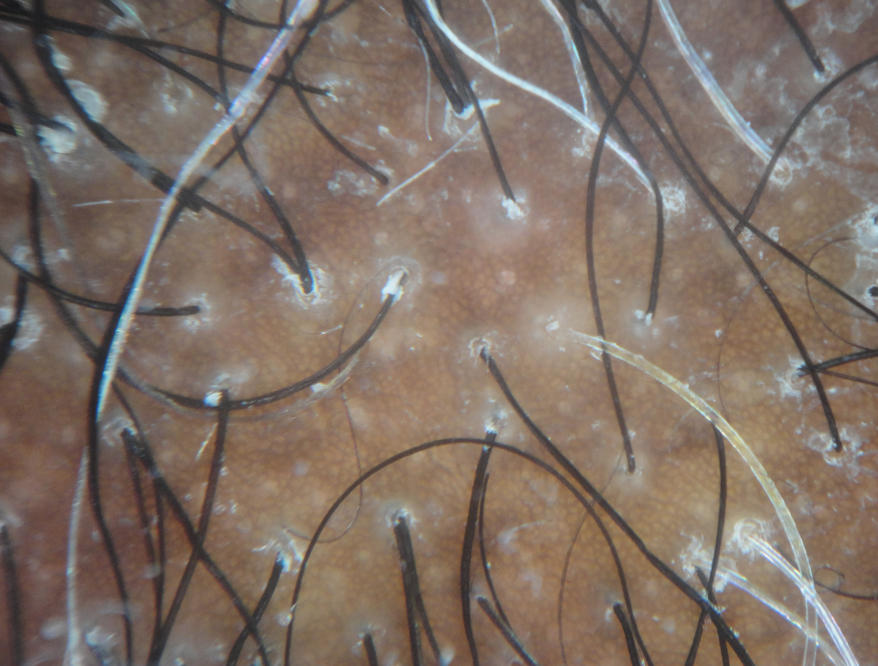
TNF-α antagonists have been associated with paradoxical psoriasiform, lichenoid, eczematous, granulomatous, and acneiform eruptions. Lichenoid reactions specifically are uncommon but are an emerging cutaneous adverse effect. In 2010, Fernandez-Torres reported the development of lichen planopilaris in with infliximab treatment. The patient in the case was a 37-year-old man with recalcitrant plaque psoriasis who was being treated with infliximab at a dosage of 5 mg/kg every 8 weeks. However, 11 months into treatment he presented with follicular keratotic papulo-pustules, perifollicular erythema, and scaling, with progressive hair loss of the frontal and parietal regions of the scalp and eyebrows. In 2016, Jayasekera and colleagues reported the development of lichen planopilaris in a 12 year old girl treated with adalimumab for oliogarthritis. Her lesions cleared with discontinuation of the clobetasol.
b) Anti-CD20: Rituximab
Rituximab is a chimeric monoclonal antibody against the protein CD20, which is primarily found on the surface of immune system B cells. In 2011, Erras and colleagues published a report in the European Journal of Dermatology of a patient with juvenile arthritis treated with rituximab who experienced complete resolution of co-existening lichen planopilaris.
c) Anti-IL-12 and anti-IL-23 monoclonal antibody: Ustekinumab
In 2015, Weber published a report of a patient with LPP treated with ustekinumab over a 10 months period without evidence of any benefit
d) Anti-LFA1: Efalizumab
To the best of my knowledge, there are no reports of lichen planopilaris with this group of agents no evidence of a treatment benefit with these agents.
e) Anti-CD2 antibody: Siplizumab
To the best of my knowledge, there are no reports of lichen planopilaris with this group of agents no evidence of a treatment benefit with these agents.
f) Anti-CD4 antibody: Orthoclone (OKTcdr4a)
To the best of my knowledge, there are no reports of lichen planopilaris with this group of agents no evidence of a treatment benefit with these agents.
g) Anti-CD25 antibodies: Basiliximab, Daclizumab
To the best of my knowledge, there are no reports of lichen planopilaris with this group of agents no evidence of a treatment benefit with these agents.
h) Anti-CD80r: Galiximab (IDEC 114)
To the best of my knowledge, there are no reports of lichen planopilaris with this group of agents no evidence of a treatment benefit with these agents.
i) Anti-IgE: Omalizumab
To the best of my knowledge, there are no reports of lichen planopilaris with this group of agents no evidence of a treatment benefit with these agents.
CATEGORY 2: Fusion Antibody Proteins
Fusion proteins, also known as 'chimeric proteins', are proteins which are created by the fusion of the receptor domain of a human protein with the constant region of human IgG. The resultant fusion protein then attaches (binds) specifically to a ligand or co-receptor. Recombinant fusion proteins have also been produced by combining human proteins with bacterial toxins. The fusion proteins most commonly used in dermatology are Etanercept, Alefacept, Abatacept, and Denileukin Diftitox. Of these four agents, only Etanercept has been studied in relationship to lichen planopilaris.
a) Etanercept
In 2009, Abbasi and colleagues reported the development of lichen planopilaris in a patient with psoriasis who was treated with etanercept. Just the year before, Garovich reported a case of LPP with etanercept in the British Journal of Dermatology.
b) Alefacept
To the best of my knowledge, there are no reports of lichen planopilaris with this group of agents no evidence of a treatment benefit with these agents.
c) Abatacept
To the best of my knowledge, there are no reports of lichen planopilaris with this group of agents no evidence of a treatment benefit with these agents.
d) Denileukin Diftitox
To the best of my knowledge, there are no reports of lichen planopilaris with this group of agents no evidence of a treatment benefit with these agents.
CATEGORY 3: Recombinant human cytokines and growth factors
This category consists of water soluble non-immunoglobulin proteins and glycoproteins produced by a wide variety of cells. A variety of immune stimuli lead to their production and release. Recombinant cytokines or cytokine antagonists are manufactured by recombinant DNA technology have been used as immunomodulators for malignant and inflammatory skin conditions. The principal recombinant cytokines used in dermatology are interferon α (IFNα), Interferon γ (IFNγ), Interleukin 1 Receptor antagonist (IL1Ra), Interleukin 2 (IL-2), Interleukin 4 (rhIL-4), Interleukin 10 (rhIL-10), Interleukin 11 (rhIL-11), Granulocyte macrophage colony stimulating factor (GM-CSF), Platelet derived growth factor (PDGF).
To the best of my knowledge, there are no reports of lichen planopilaris with this group of agents no evidence of a treatment benefit with these agents.
REFERENCE
Abbasi NR, et al. Lichen planopilaris noted during etanercept therapy in a child with severe psoriasis. Pediatr Dermatol. 2009
Fernández-Torres R, et al. Infliximab-induced lichen planopilaris. Ann Pharmacother. 2010.
Garcovich S, et al. Onset of lichen planopilaris during treatment with etanercept. Br J Dermatol. 2008
Jayasekera PS, et al. Case Report of Lichen Planopilaris Occurring in a Pediatric Patient Receiving a Tumor Necrosis Factor α Inhibitor and a Review of the Literature. Pediatr Dermatol. 2016 Mar-Apr.
McCarty M, et al. Lichenoid Reactions in Association with Tumor Necrosis Factor Alpha Inhibitors: A Review of the Literature and Addition of a Fourth Lichenoid Reaction. J Clin Aesthet Dermatol. 2015Erras S, et al. Rapid and complete resolution of lichen planopilaris in juvenile chronic arthritis treated with rituximab. Eur J Dermatol. 2011 Jan-Feb.
Webster G. Failure of lichen planopilaris to respond to ustekinumab. Dermatol Online J. 2015.