Manuka Honey for Treating Folliculitis Decalvans
Antibacterial Properties of Manuka Honey May Provide Benefits in Treating Folliculitis Decalvans
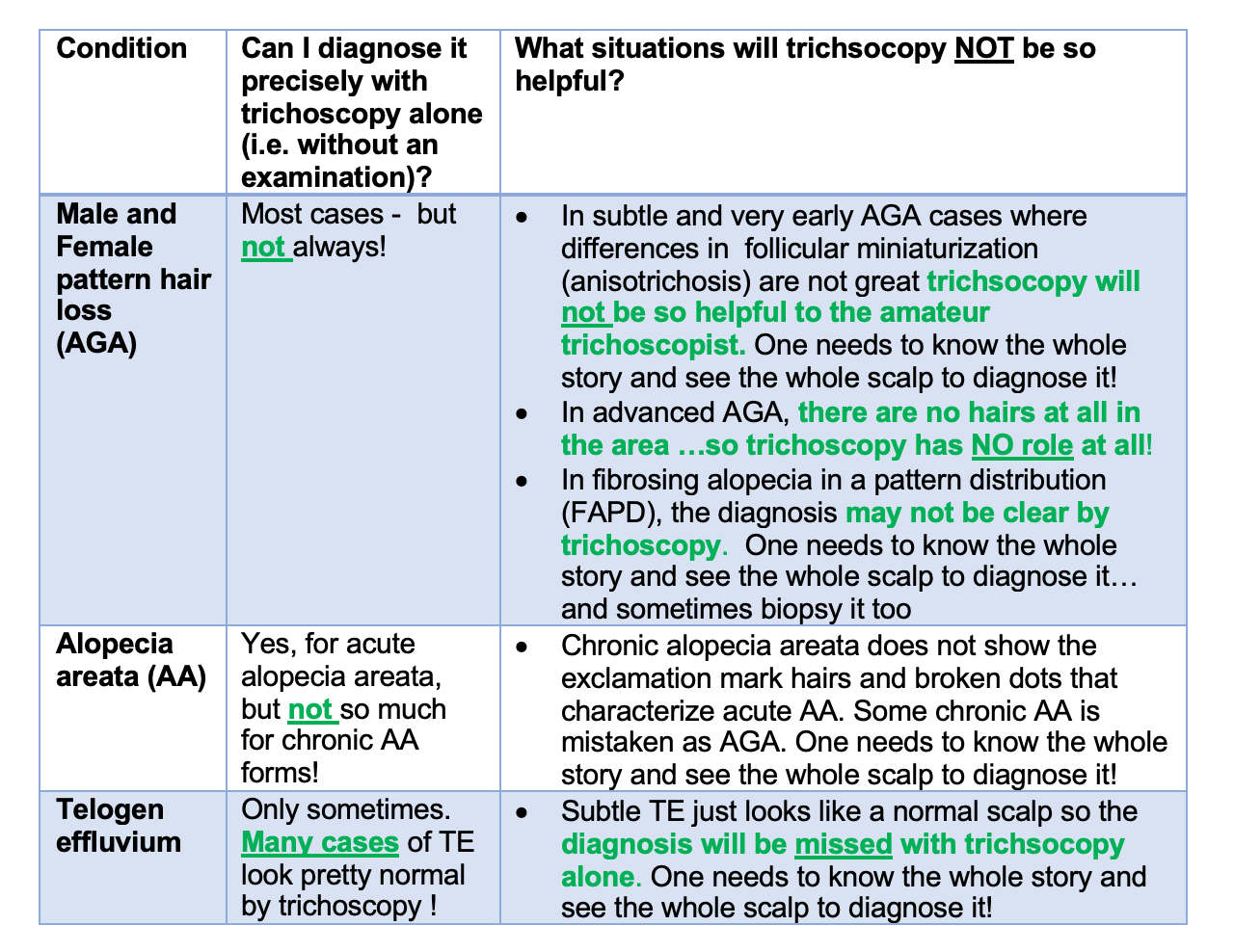
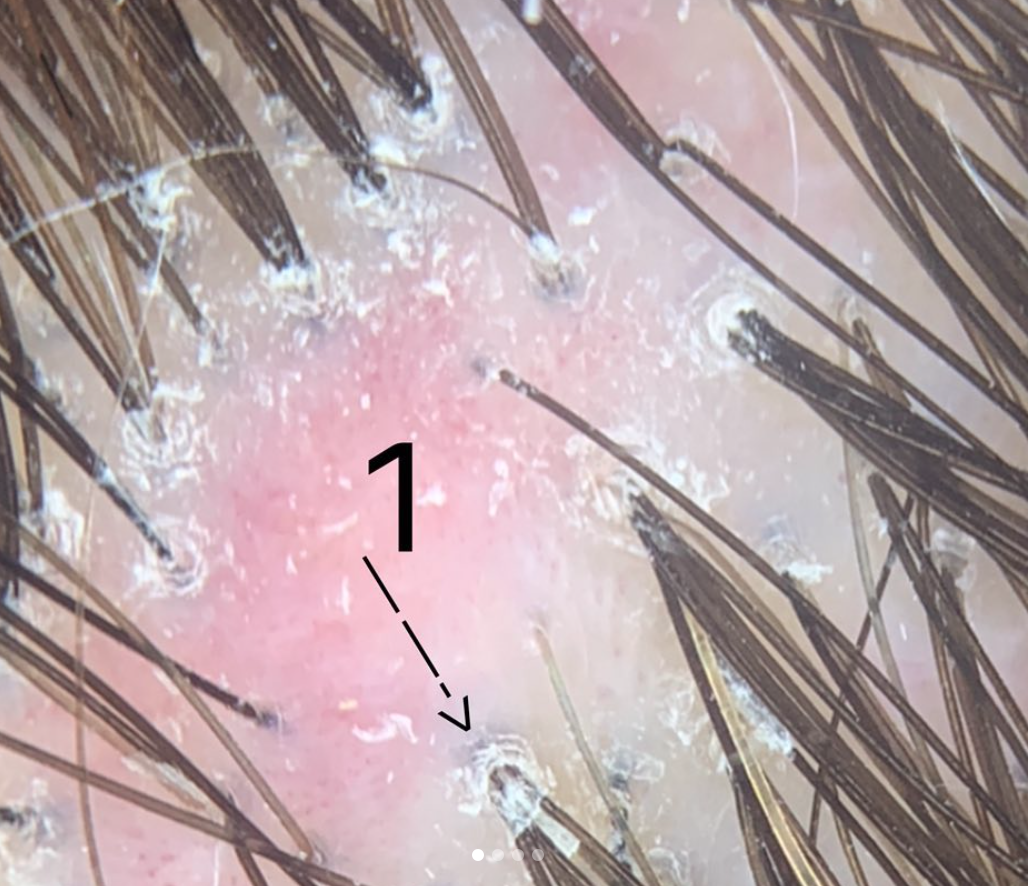
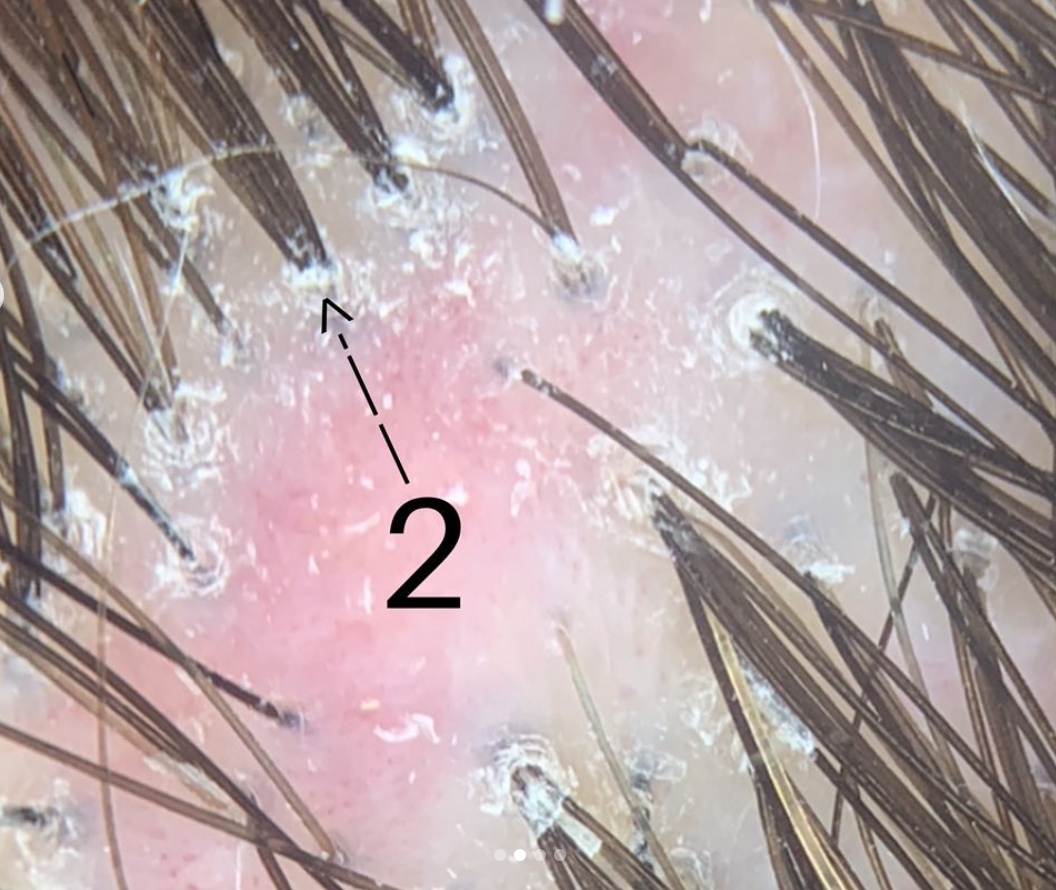
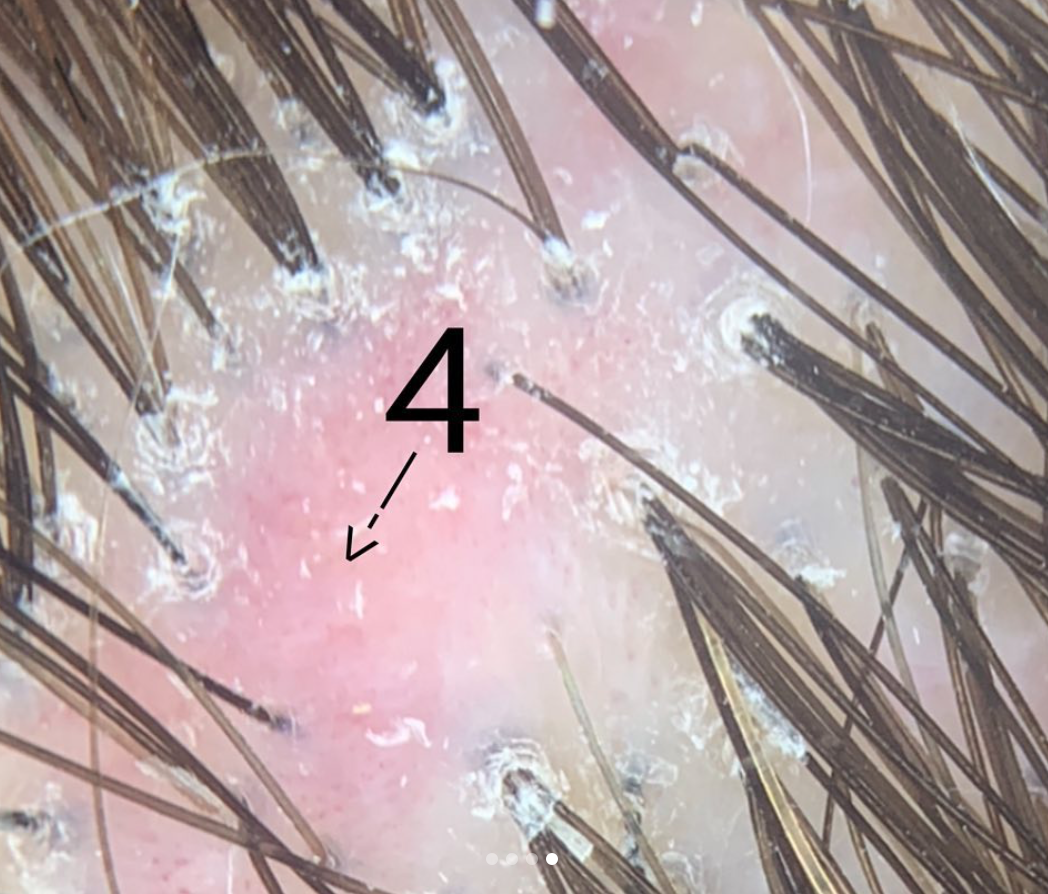
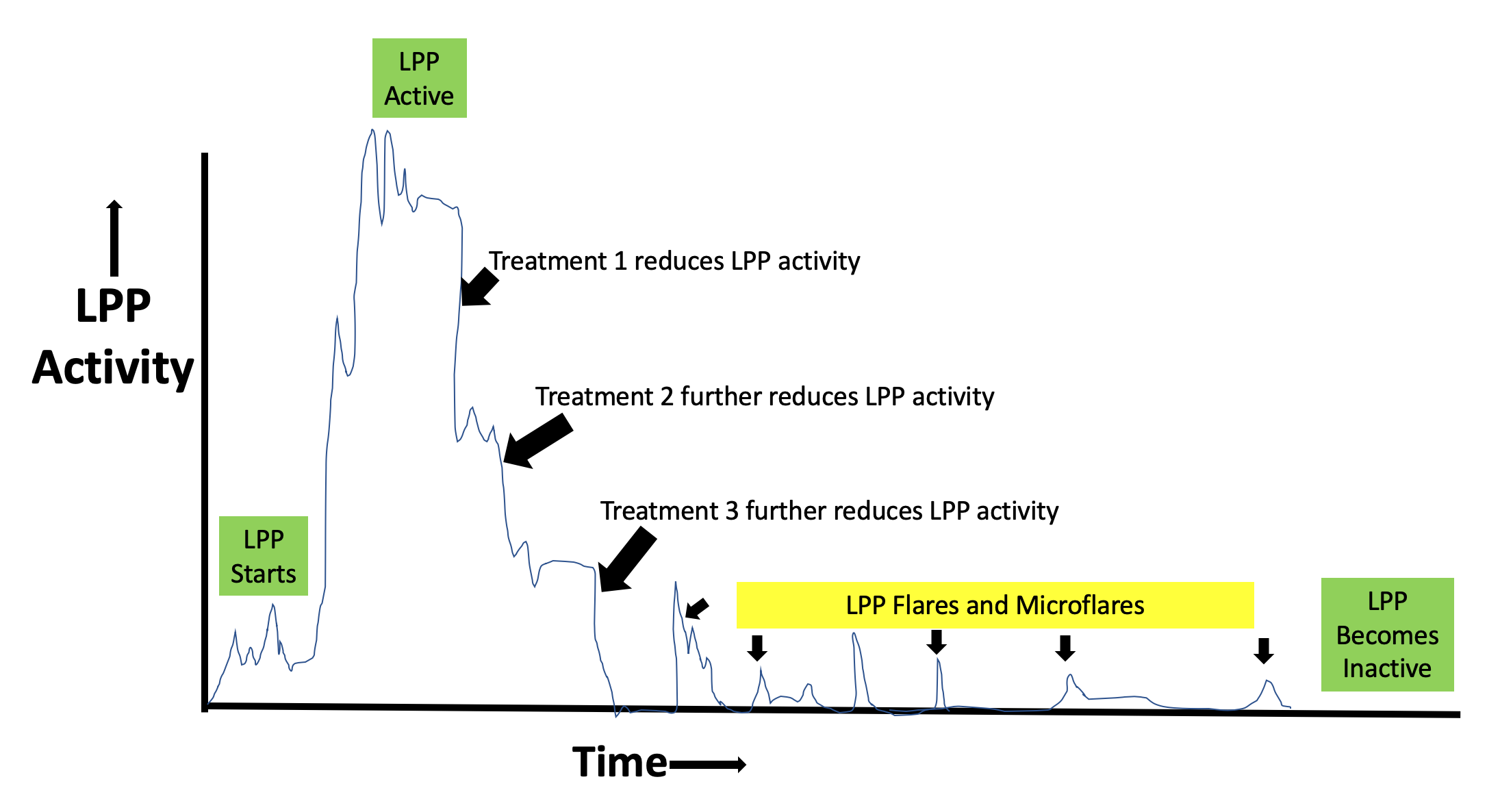
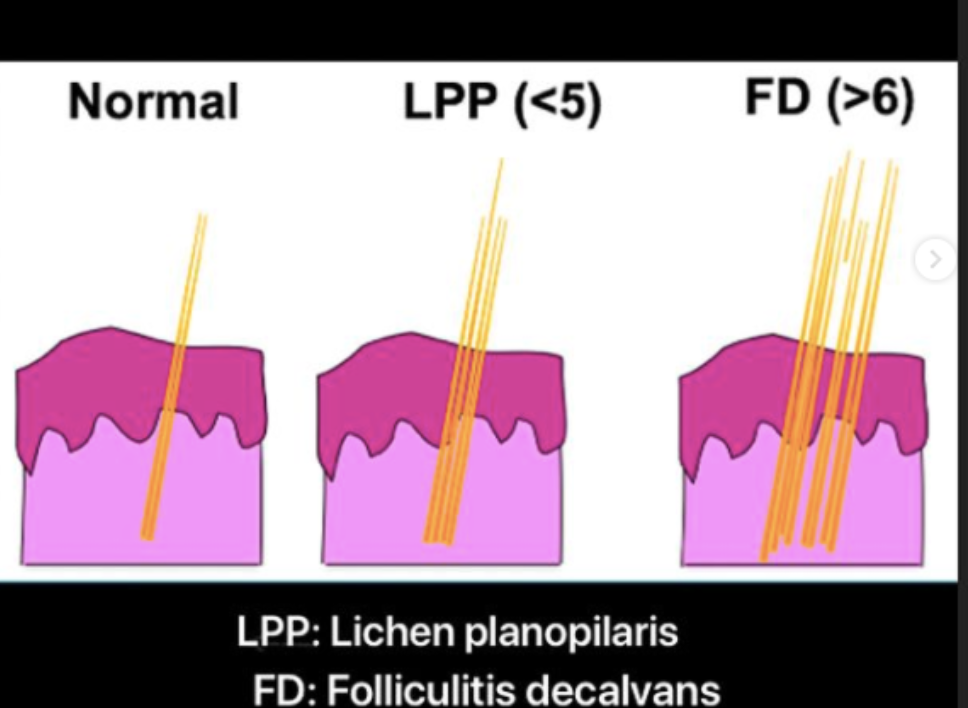
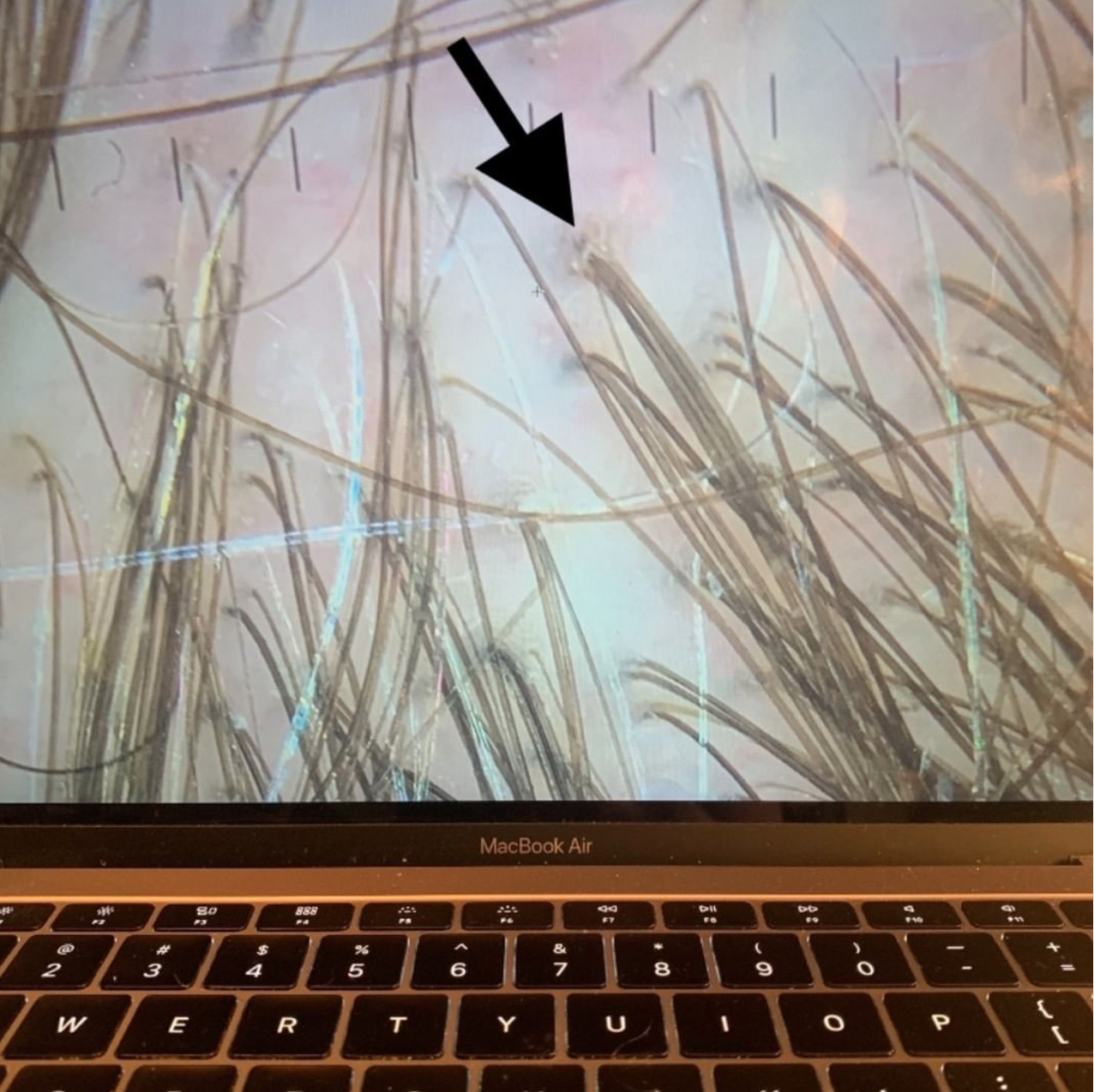
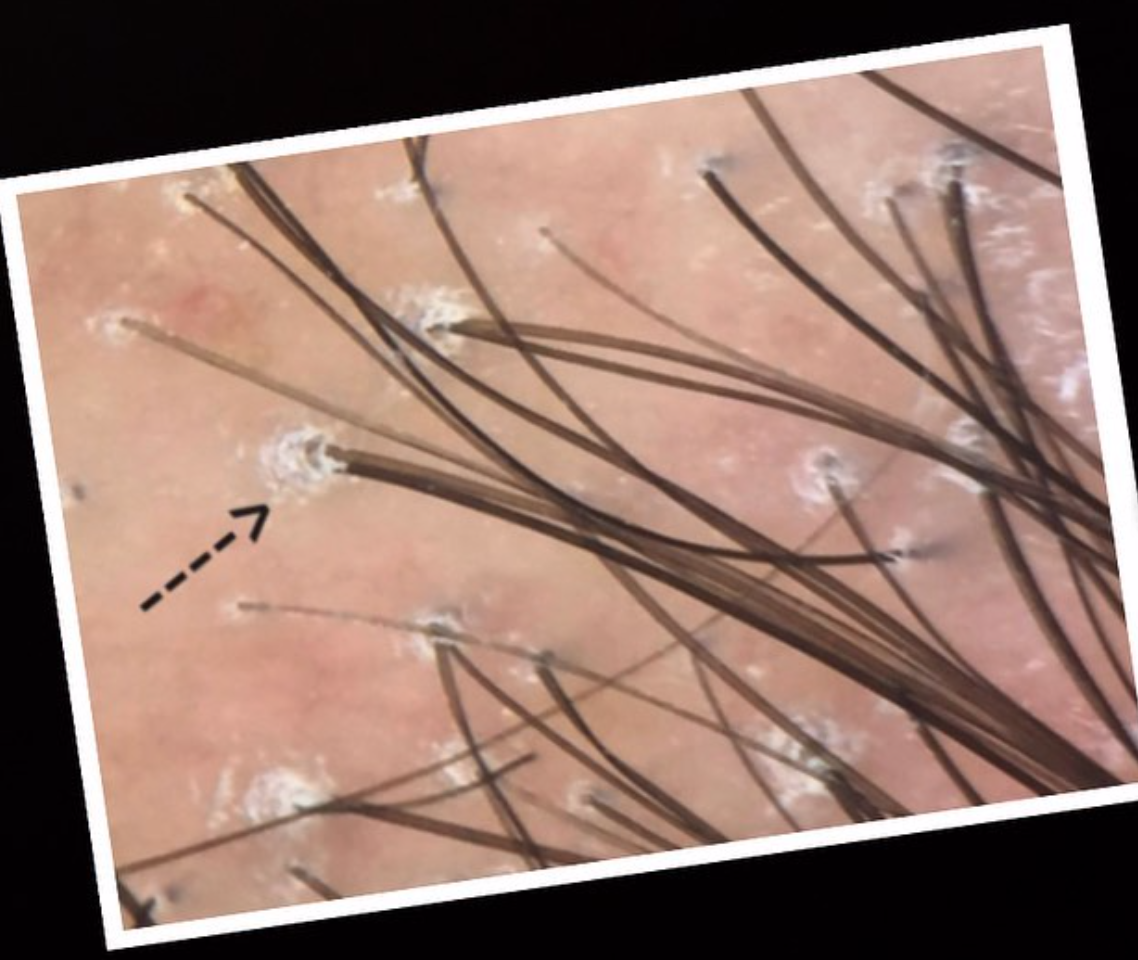
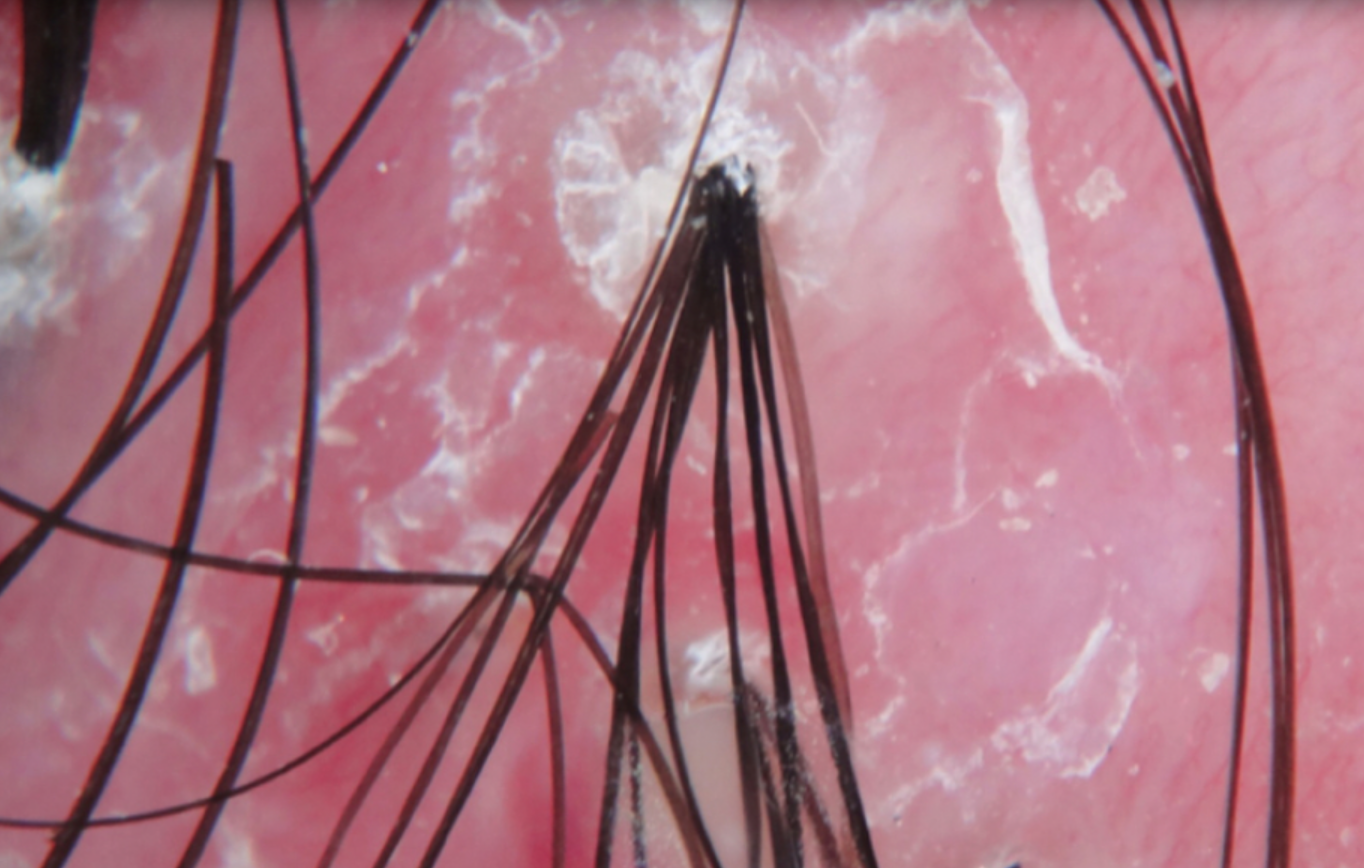
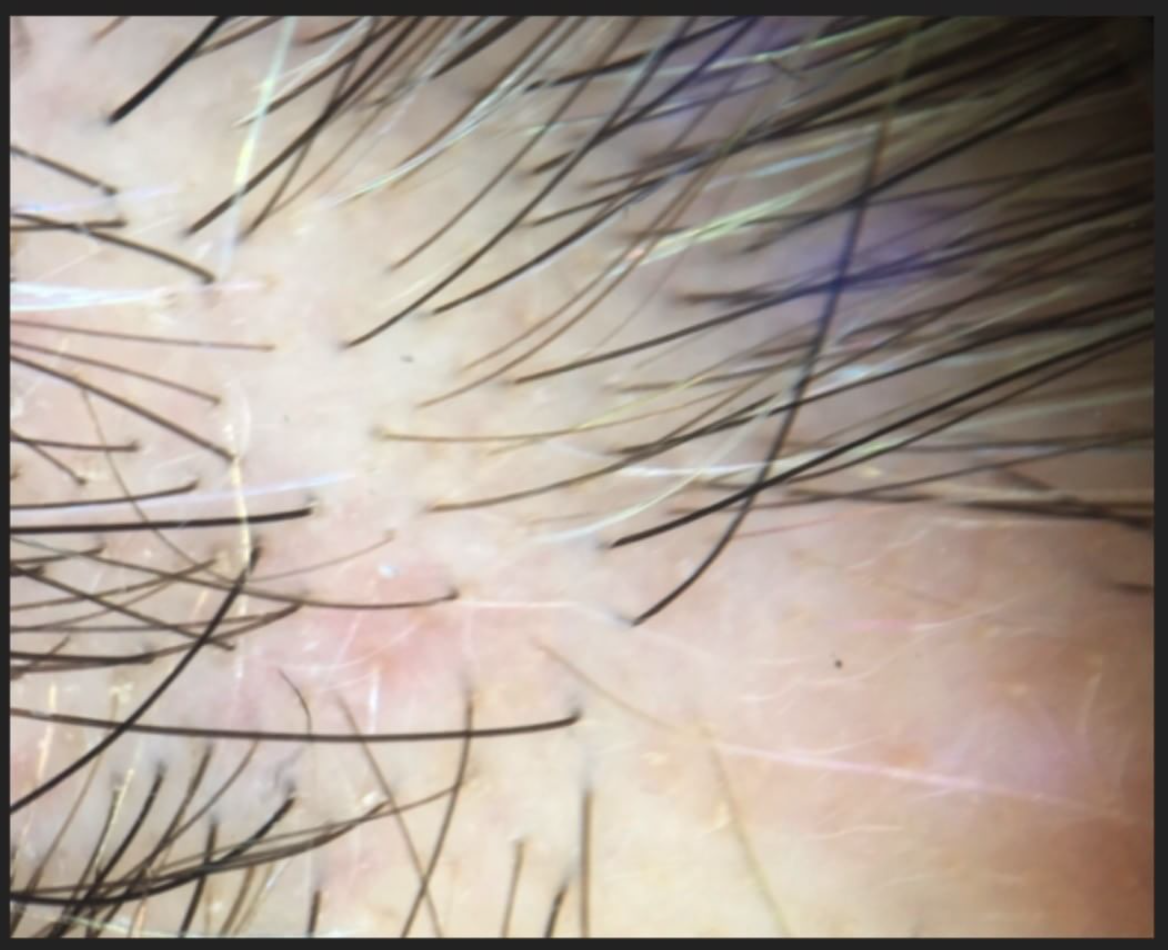
Folliculitis decalvans (FD) is a scarring alopecia that affects both men and women. FD is less common than some of the other scarring alopecias like lichen planopilaris and central centrifugal cicatricial alopecia. The cause of FD is not completely know although a role for bacteria has been postulated. Bacteria such as Staphylococcus aureus frequently are found in the scalp of patients with folliculitis decalvans. Eradication of bacteria with antibiotics, isotretinoin and other treatments frequently is associated with improvement of the disease.
A preliminary report proposes that Manuka honey may have benefits in the treatment of folliculitis decalvans
In 2019, a dermatology group in Boston reported a patient with folliculitis decalvans whose disease improved with use of topical Manuka honey applied to the scalp. Manuka honeyis well known to wound care professionals. In fact, 17 clinical trial s involving almost 2000 patients have suggested Manuka honey helps wounds heal. Manuka honey has antibacterial properties – perhaps due to its low pH, and other plant based and hydrogen peroxide based ingredients. A 1999 paper by Cooper and colleagues showed that Manuka honey killed Staph aureus bacteria in wounds.
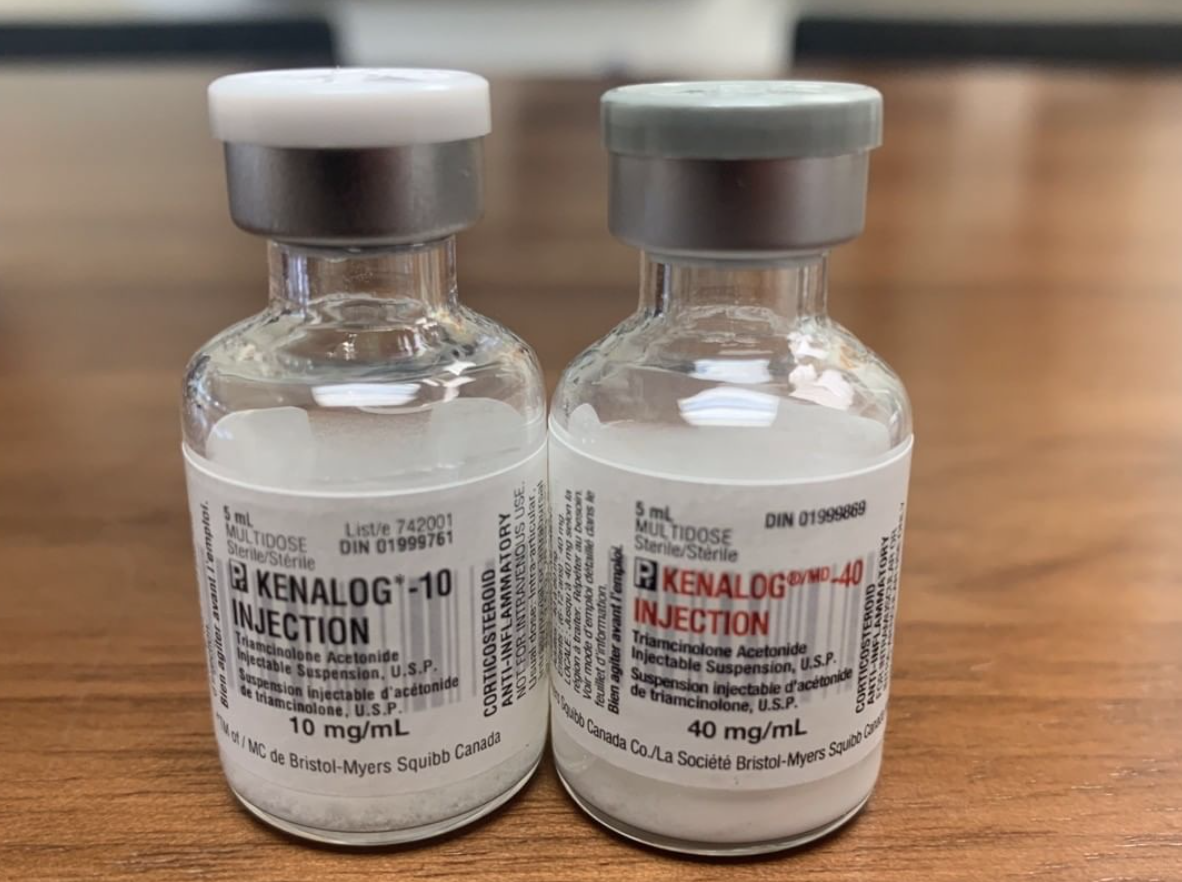
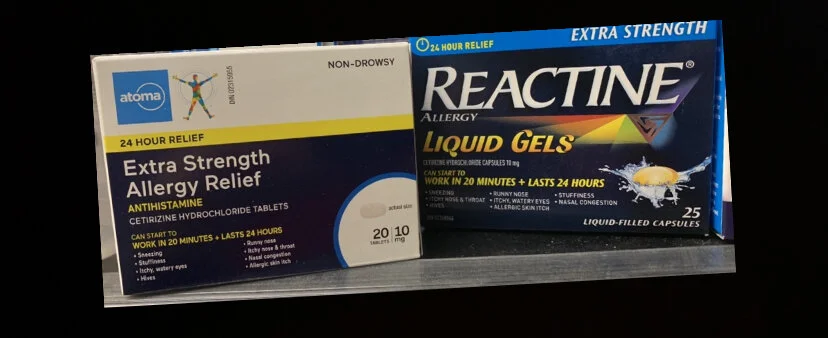
The patient in the 2019 paper was a 20 year old male who had used a considerable number of treatment before he started applying manuka honey to his scalp. These treatments included steroid injections, clobetasol lotion, prednisone, minocycline, doxycycline and isotretinoin. Some of these treatments were actually quite helpful for the young man – however he had to stop because of some side effects of these treatment.
The patient decided to start applying Manuka honey to his scalp after about 1 month into a course of the oral antibiotic cephalexin. As he continued on both cephalexin and topical honey and found that after an additional 4 weeks of both treatments the scalp had improved considerably. 6 months later he stopped cephalexin. His disease eventually flared again and the man used honey alone to settle down his disease.
Summary/Conclusion
This is an interesting paper. It doesn’t definitively prove Manuka honey helps FD but it hints that it might have a role. We also can’t rule out that the patients long term use of antibiotics and other treatments (like steroids) and isotretinoin have reduced disease activity that makes Manuka honey more likely to help. Nevertheless, this is an interesting paper that hopefully fuel more research in manuka honey.
Reference
Yeh et al. Resolution of folliculitis decalvans with medical honey. Dermatology Online Journal 2019;. 25(8);
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.