Seborrheic Dermatitis Risk Factors: Altitude and UV Radiation
Altitude and UV Radiation
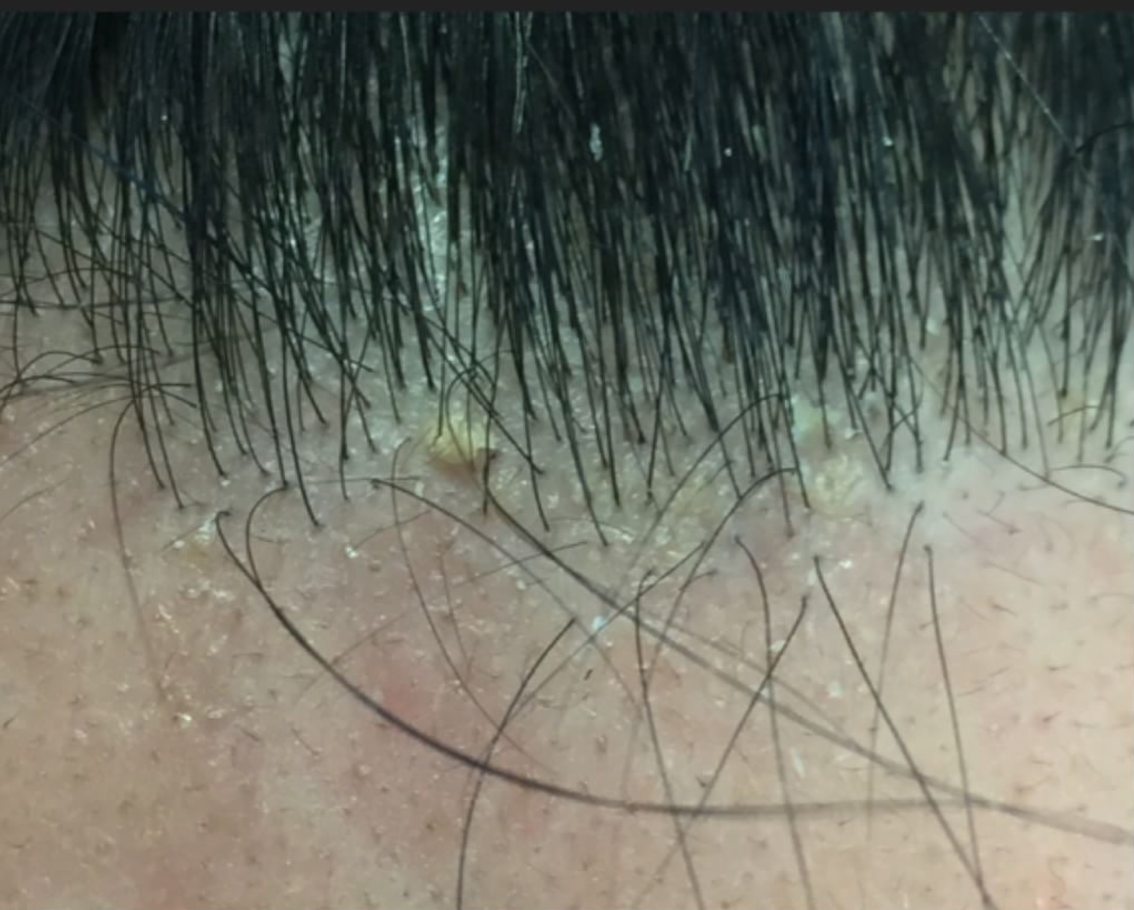
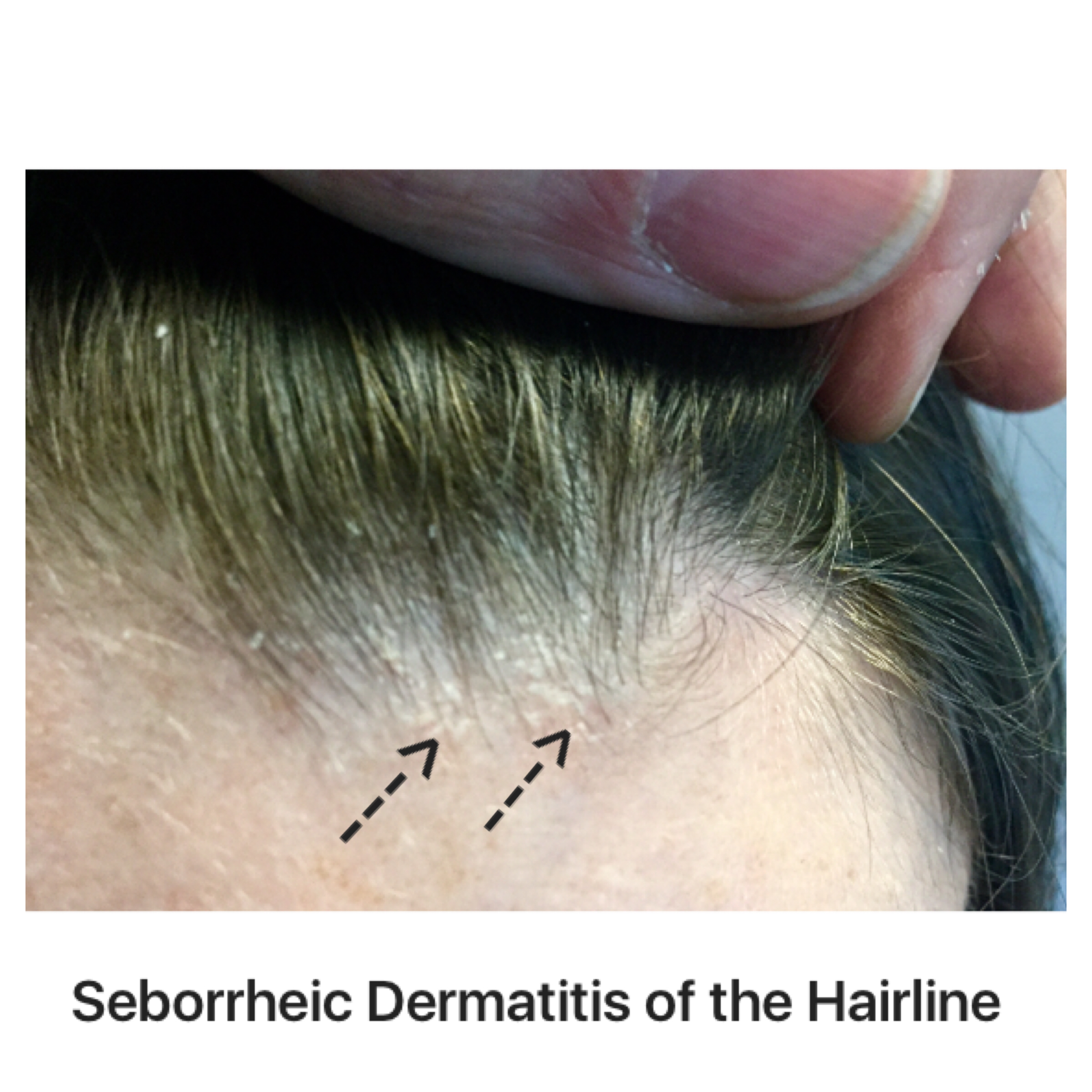
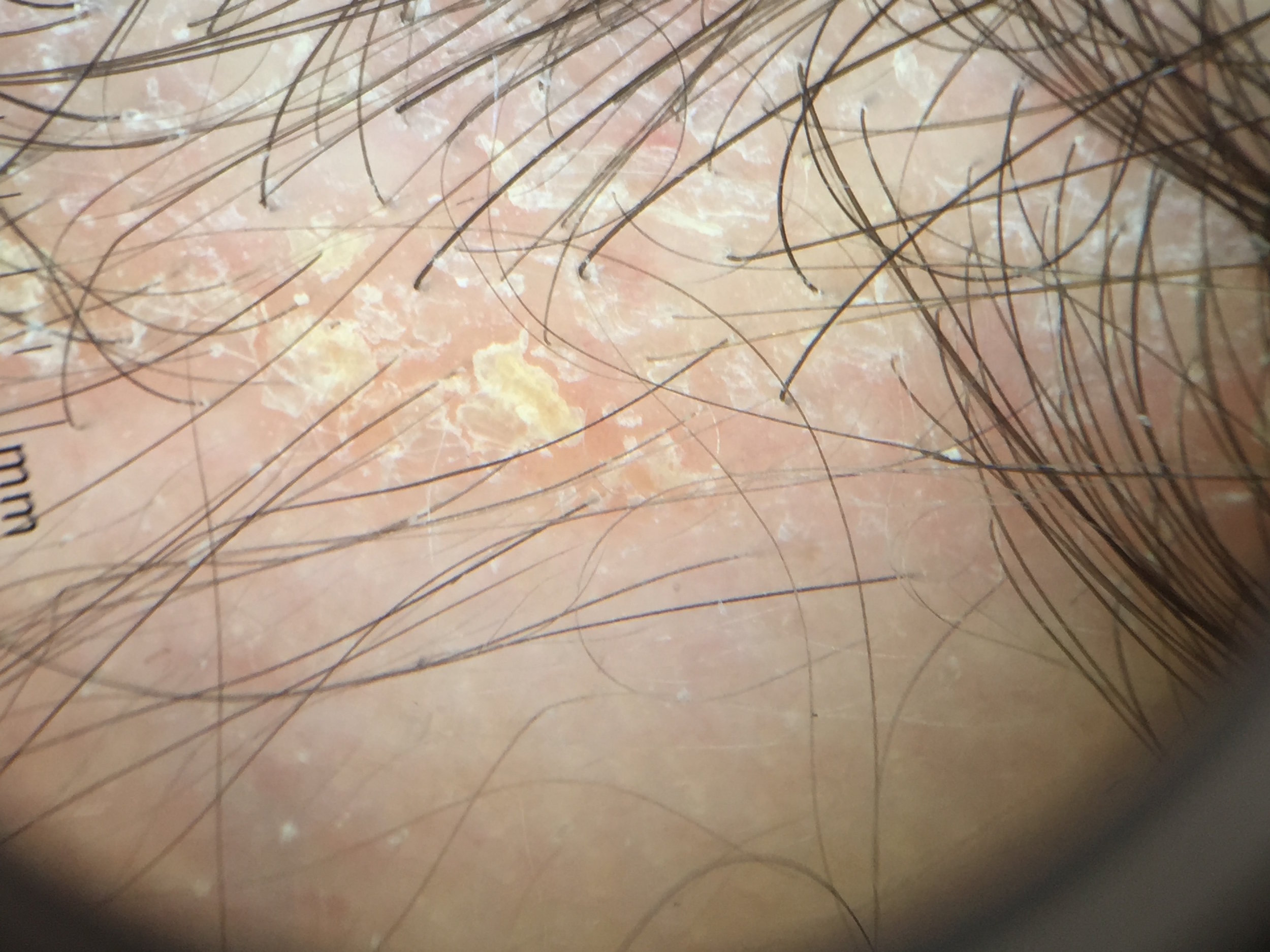
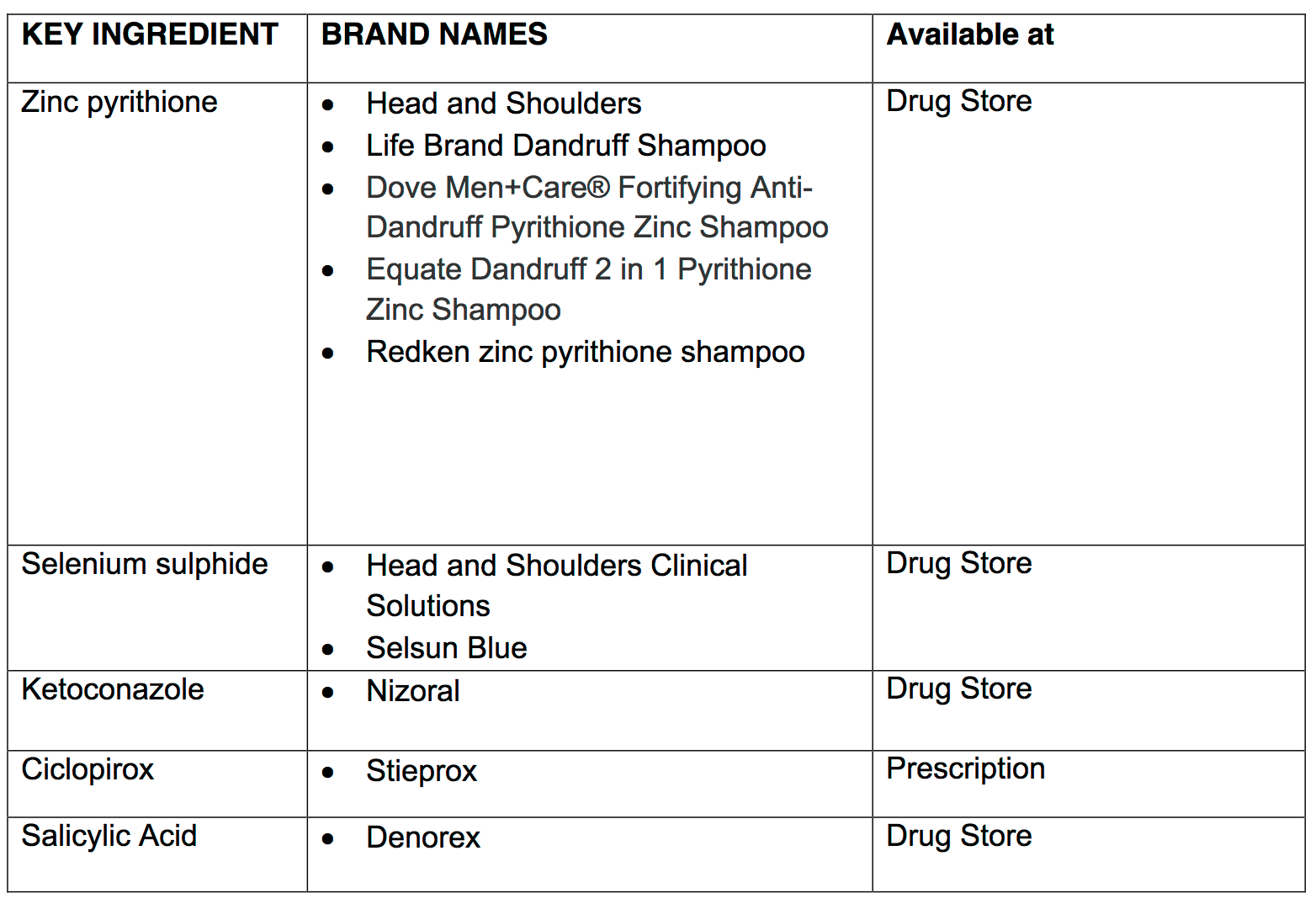
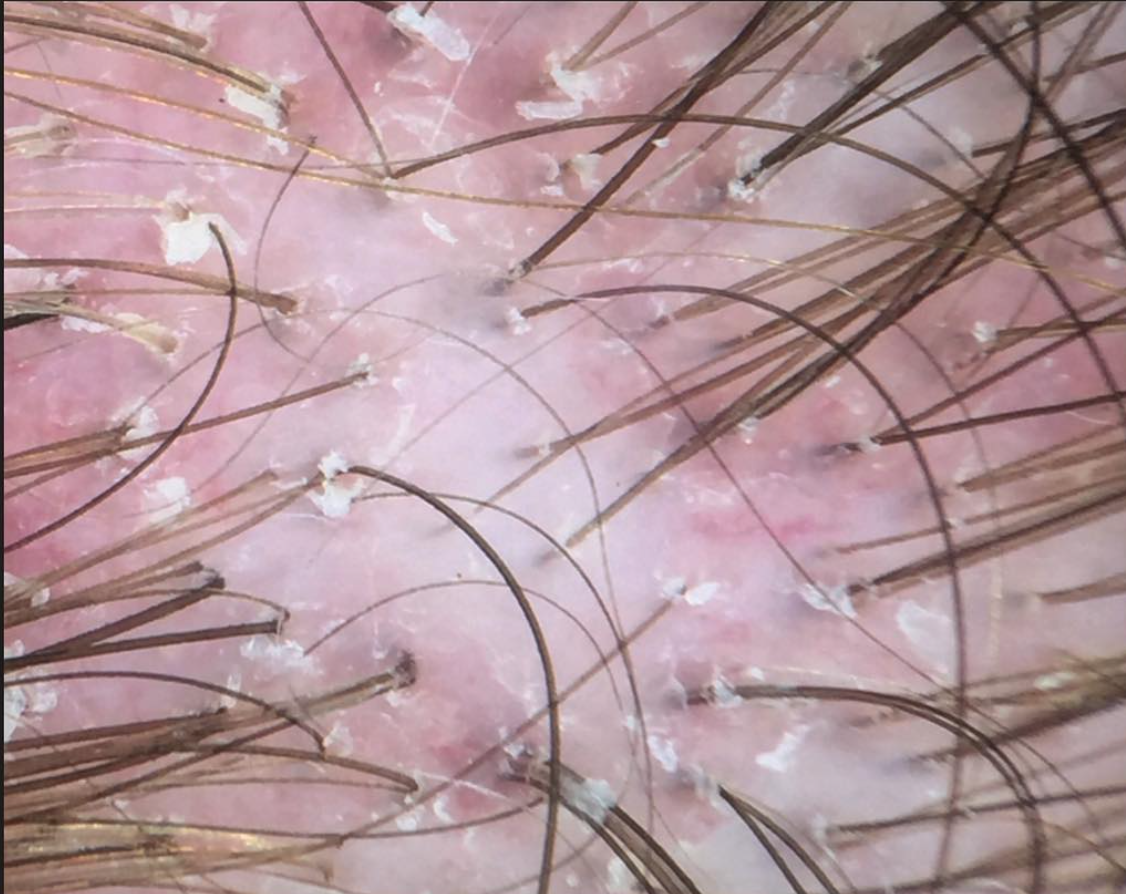
Seborrheic dermatitis is a common condition that can affect the scalp (where it causes an itchy, red and greasy scalp) but can also affect the eyebrows, face, chest as well as other areas too. A yeast known as Malassezia has an important role.
There are many factors that are known to increase one’s risk of developing seborrheic dermatitis. For example, stress, age, heat, humidity, depression, Parkinson’s disease, head injury, neurological disease, HIV and UV radiation all increase the risk of SD. Other risks include acne, lighter skin, higher body fat content.
It’s clear that immunosuppression can affect SD. This is especially true in patients with HIV/AIDS. But we also see the effect of immunosuppression with ultraviolet radiation which is also a form of immunosuppression. Studies have shown that some individuals experience flares with intense UV radiation exposure.
High altitude may be a risk factor for seborrheic dermatitis.
An interesting study conducted in 2000 looked at the risk of SD in 283 mountain guides from 3 different counties who have a high occupational exposure to UV radiation. 16.3% mountain guides when examined clinically were found to have SD and these rates were similar across the 3 countries. This number is higher than the 3-5 % rate of SD in the general population. These studies suggested that UV-induced immunosuppression due to occupational sun exposure as a pathogenetic factor in SD.
Reference
Moehrle M, et al. High prevalence of seborrhoeic dermatitis on the face and scalp in mountain guides.
Dermatology. 2000
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.