Scalp Burning: Many reasons but diagnosis is essential
Scalp Burning: Before talking treatment, talk diagnosis
In our clinic, many patients present with concerns about scalp burning. There are many reasons for scalp burning and the precise treatment depends entirely on the diagnosis of the burning. A carefully obtained history, along with an examination of the scalp is needed. Some patients with burning also have itching and some have pain.
Causes of Scalp Burning
1. Diseases/Disorders of the scalp
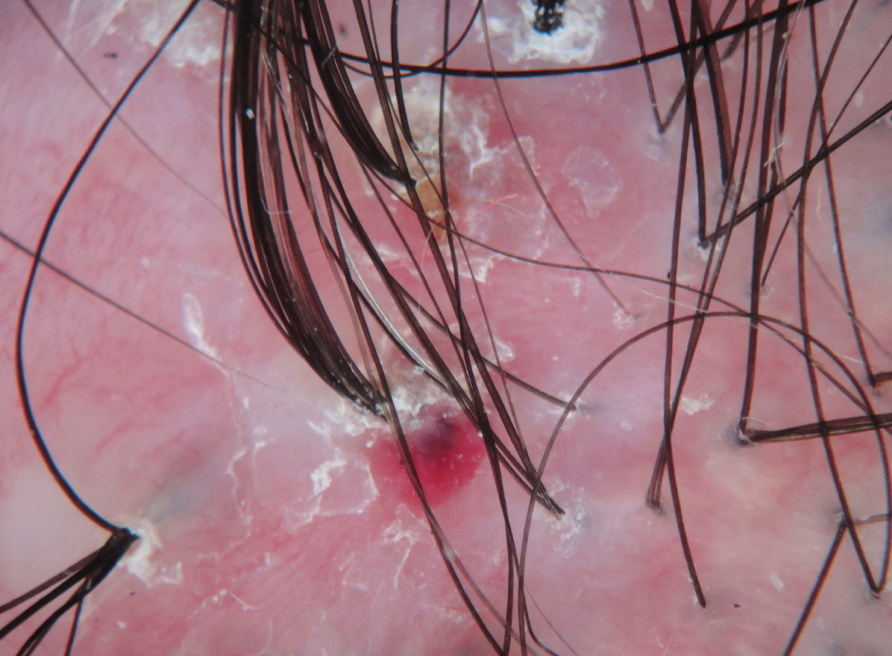
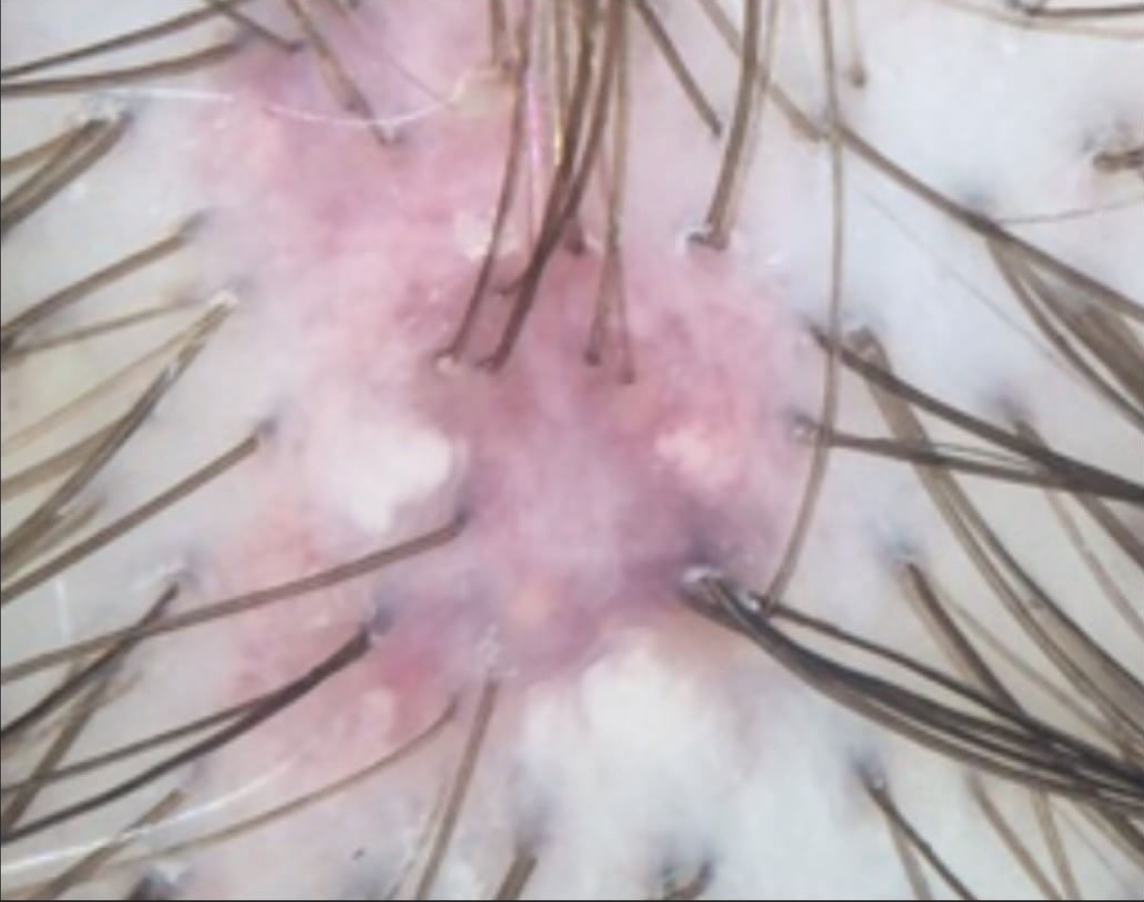
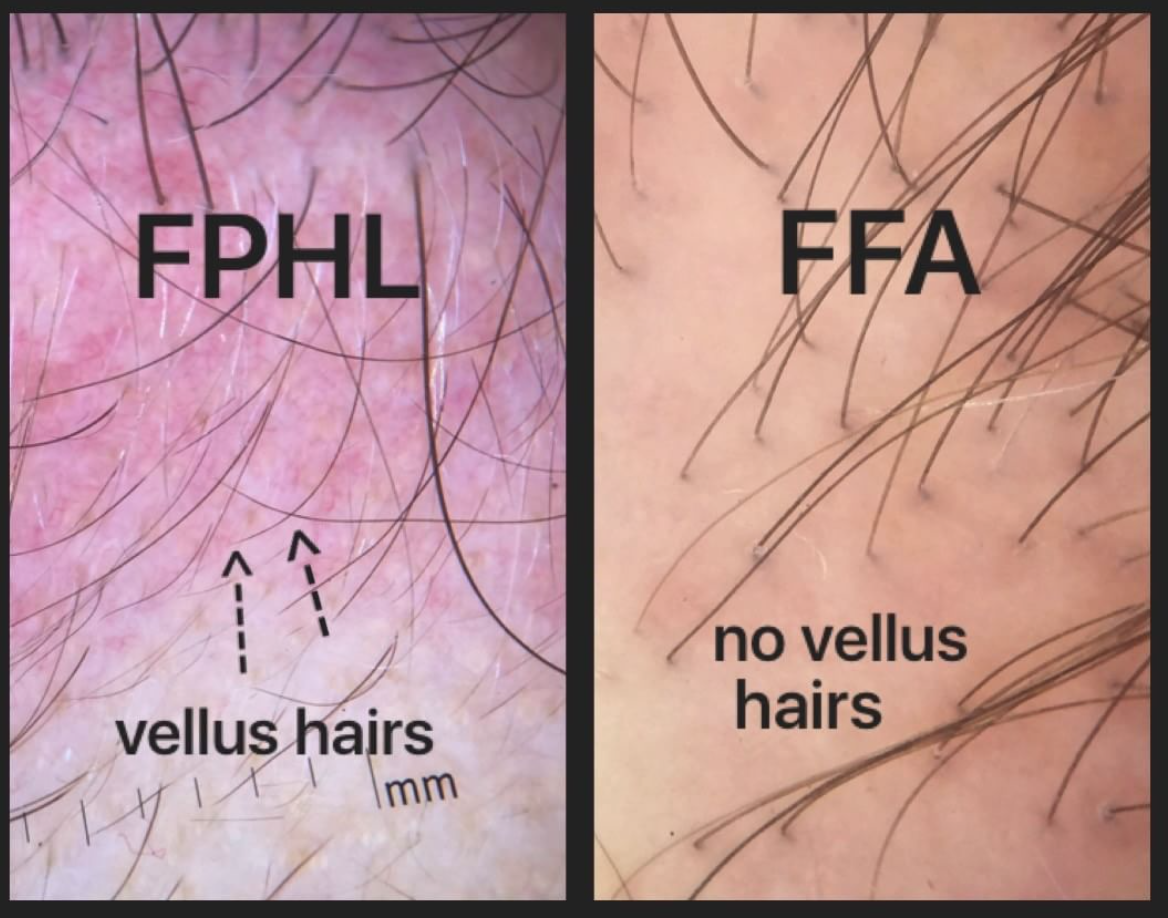
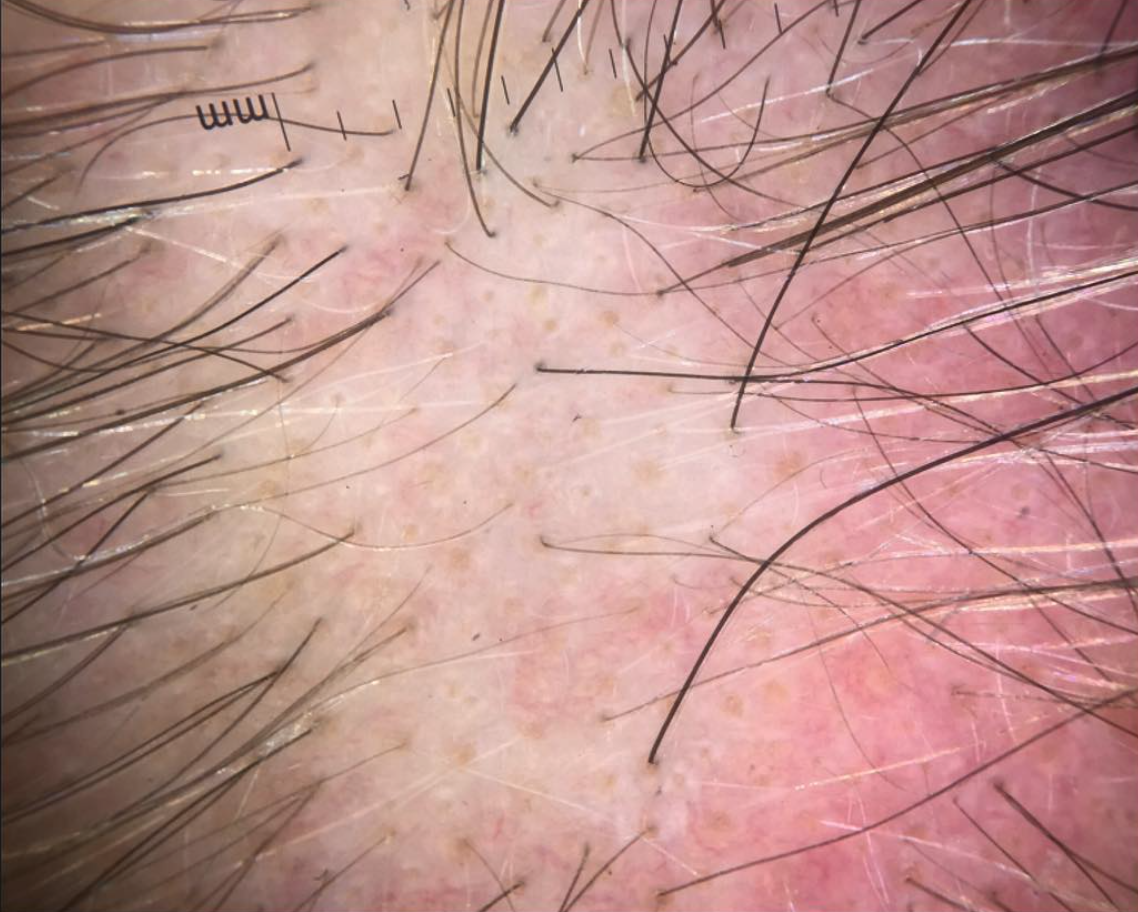
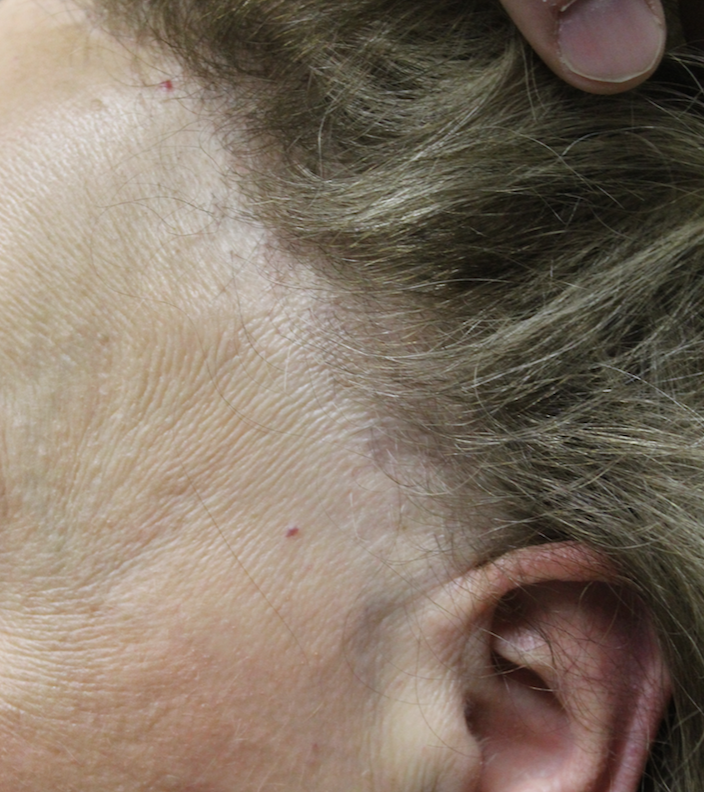
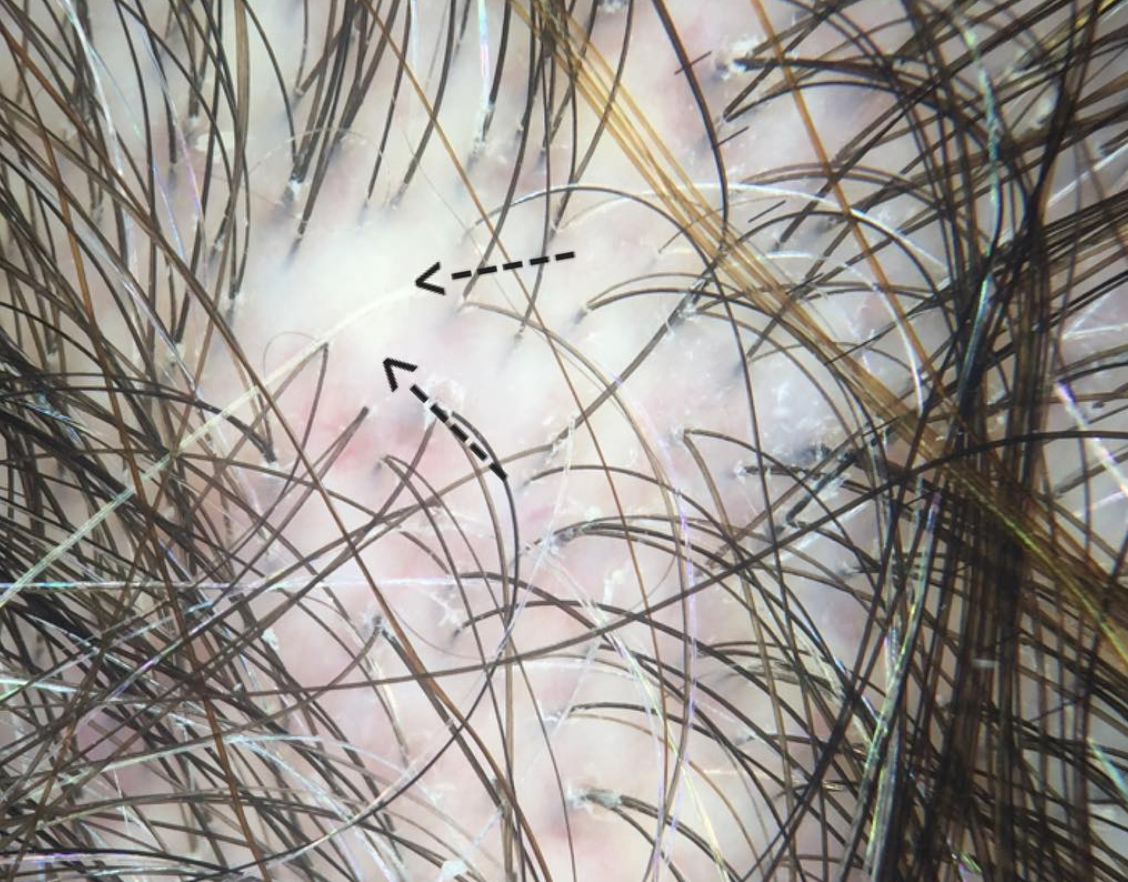
Individuals with scalp burning needs a thorough examination to evaluate for underlying scalp disease. A variety of inflammatory scalp disorders can trigger burning including scalp psoriasis, seborrheic dermatitis, scarring alopecia, dermatomyositis, tinea capitis, sunburns, irritant and allergic contact dermatitis. Common hair loss conditions such as androgenetic alopecia, telogen effluvium and scarring alopecia are also associated with burning in some cases.
2. Dysesthesias
The scalp dysesthesias, as described by Hoss and Segal in 1998, are a group of conditions that give physical symptoms in the scalp without any other unusual findings at the time of examination (normal scalp examination). In addition to scalp burning, many patients with scalp dysesthesias have itching and pain.
The cause of scalp dysesthesias is not clear. One study (reference below) suggested that a high proportion of women with scalp dysesthesias had cervical spine disease. It seems that patients worsen with stress and improve with anti-depressants (venlafaxine, amitrytyline). Many respond to topical or oral gabapentin.
The burning scalp syndrome (similar to burning mouth syndrome) is a variant of scalp dysesthesia. Sensitive scalp syndrome may also be as well.
3. Depression and Other Psychological Issues.
There is a well known relationship between the brain and the skin and this has been referred to as the 'brain-skin' axis. Stressful life events are a well known trigger to scalp burning. Burning is more common in patients with a host of psychological and psychiatric diagnoses including anxiety, depression, post traumatic stress disorder, schizophrenia.
4. Drugs
Drugs can trigger scalp burning, both topical drugs and oral medications. Topical medications containing alcohol are frequent triggers or scalp burning. Topical calcipotriol, topical steroids, and a host of anti-dandruff shampoos can trigger burning. Oral medications, including cyclophosphamide can trigger scalp burning.
5. Damaged Nerves and Small fiber neuropathies
Scalp burning may be a result of damage to nerves. As mentioned above, cervical spine disease may be one such condition. But diabetes, multiple sclerosis, and stroke can all give scalp symptoms.
Many issues affecting the tiny nerves of the scalp can cause scalp burning. This is seen in many of the autoimmune diseases including Sjogren’s syndrome.
6. Sleep Deprivation
Sleep deprivation has been associated with many cutaneous symptoms including scalp burning.
Treatment for Burning Scalp
The treatment of burning scalp will depend on the diagnosis. For patients with scarring alopecia, treatments such as topical steroids, steroid injections and oral anti-inflammatory mediation such as doxycycline or hydroxychloroquine will frequently help stop the scarring alopecia itself as well as the burning. For burning due to psoriasis, a variety of topical steroids, topical vitamin D analogues can help. The scalp dysesthesias are frequently more challenging to treat but options include topical steroids, oral gabapentin, topical gabapentin, oral amitryptyline, and topical capsaicin. Avoiding harsh shampoos is important.
Breathing, exercise and scalp exercises are also important as outlined in prior posts.
Conclusion
In summary, there are many reasons for a patient to present with concerns about burning scalp. A careful and detailed history along with a scalp examination is important. Many times, a scalp biopsy is needed.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.