What cancers metastasize to the scalp?
Lung cancer tops the list of cancers that metastasize to the scalp
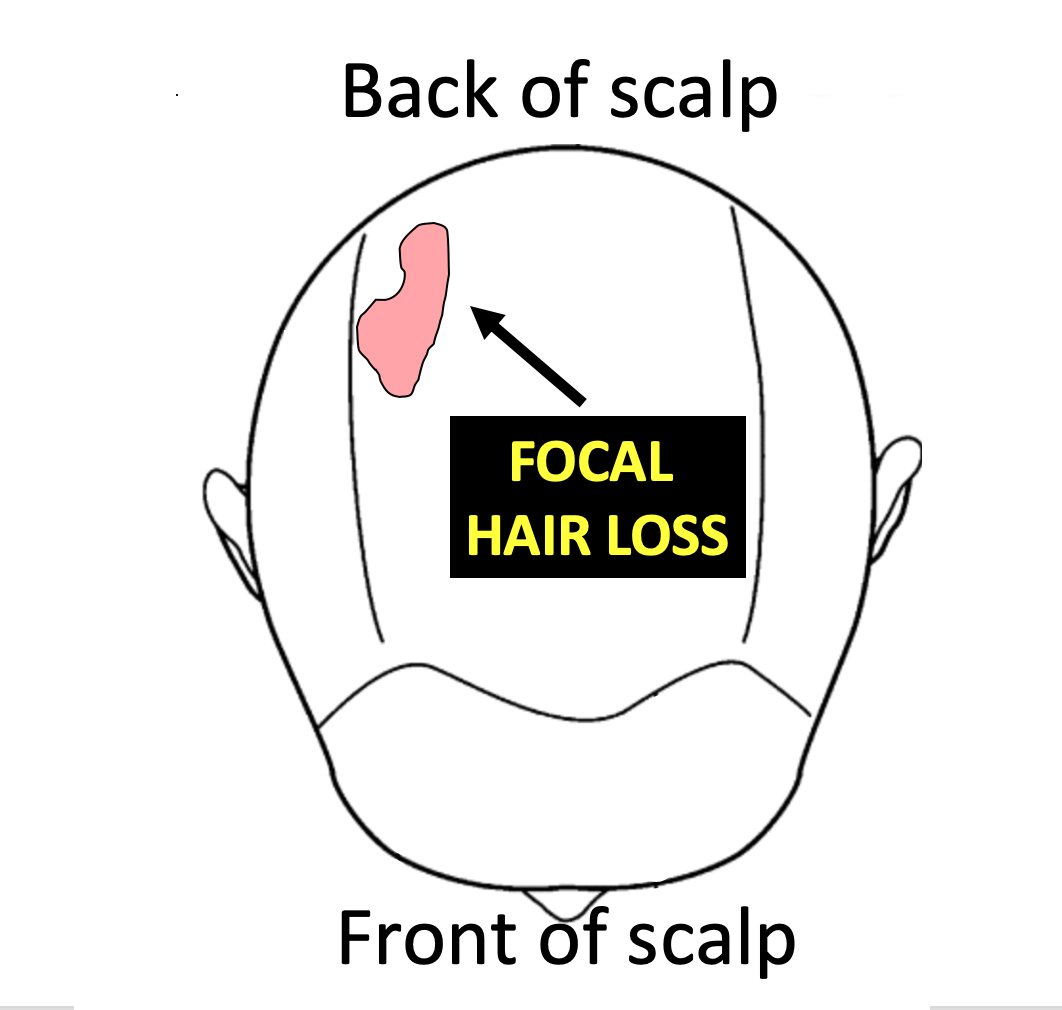
Focal alopecia refers to hair loss in a single area of the scalp. Common causes of focal alopecia include alopecia areata, tine capitis, infections, trauma, trichotillomania. Cancer is another cause of focal alopecia - albeit an uncommon one.
Scalp metastases refer to cancer the started in another organ and then the cancer spread to other parts of the body, including the scalp. Less than 2 % of patients that are known to have metastatic cancer will experience scalp metastases.
What are the most common cancers that metastasize to the scalp?
Lung cancer is the most common cancer that is associated with scalp metastases. Of all metastases to the scalp, lung cancer is the most common at 24 % followed by colon (11 %), liver (8 %) and breast (8%). Kidney and ovary remain other causes on the list. In 30 % of cases, the exact origin can’t be precisely determined. There are many types of ‘lung cancer’ and it remains debated as to which of the types is really the most likely contributor to scalp metastases (adenocarcinoma, large cell, small cell, squamous).
What are the clues that an area of hair loss may actually represent a metastasis?
Scalp metastases can be challenging to diagnose in the early stages. Sometimes they aren't large and sometimes they get overlooked. They may appear as papule or nodules, or firm indurated plaques or ulcers or as an area closely mimicking alopecia areata. They may simply appear as an area that looks like an infection. In many cases, they are red from dilated blood vessels - and sometimes hemorrhagic from localized blood clots in the area. “Alopecia neoplastica” is a term that refers to hair loss associated with destruction of hair follicles. It is accompanied by red, indurated skin with dilated blood vessels and sometimes ulceration. In most cases, alopecia neoplastica represents hematologenous spread (spread in the blood stream) of a breast cancer. In some cases of metastastic scalp lesions, the areas of involvement are associated with no symptoms which in turn adds to the delay in diagnosis. In fact, there can be a delay in diagnosis for many patients with some studies showing a delay in proper diagnosis of 4–10 months following the time they are first noticed.
The identification of a scalp metastasis can rarely be the very first indication that the patient has a cancer inside the body. This is not common and in most cases it is already known that the patient has a cancer somewhere in the body. Overall, a study by Lookingbill and colleagues of 7316 cancer patients found that 0.8 % of patients had a skin lesion that represented the presenting sign of the cancer inside the body.
Key Conclusions and Summary
Scalp metastases can be challenging to diagnose in the early stages and diagnosis of a scalp metastasis ALWAYS comes from a biopsy. One can never look at a skin lesion and know with 100 % certainty that it is a metastasis from a cancer somewhere in the body. One only reaches that conclusion after a biopsy is done.
It’s often a good idea for a doctor to consider performing scalp biopsy when a patient has a focal areas of hair loss that does not improve over time - especially in patients over 45 years of age. In situations where the diagnosis is completely clear simply by examining the scalp, a biopsy is not necessary.
In general, a biopsy should at least be considered in the following situations:
1) A patient with a history of CANCER AT ANYTIME IN THE PAST who presents with a solitary area of hair loss (i.e. affecting a single localized area of the scalp).
2) A patient with CURRENT CANCER DIAGNOSIS who presents with a solitary area of hair loss (affecting a single localized area of the scalp).
3) A patient over 45 years of age who presents with a solitary LOCALIZED, RED PATCH OF HAIR LOSS ON THE SCALP that has persisted for 3 or more months.
Most patients with previous cancer diagnoses or who are dealing with cancer at the present time do not have a scalp metastasis as the reason for their hair problems when they present to the hair doctor’s office. However, it must always be on the doctor’s radar - especially when the patient has a solitary patch of hair loss (a single spot).
Persistent solitary patches of hair loss, especially when red, are extremely important to consider biopsying in anyone over 45.
Reference
Chiu CS, Lin CY, Kuo TT, et al: Malignant cutaneous tumors of the scalp: a study of demographic characteristics and histologic distributions of 398 Taiwanese patients. J Am Acad Dermatol. 56:448–452. 2007.
Frey L, Vetter-Kauczok C, Gesierich A, Bröcker EB and Ugurel S: Cutaneous metastases as the first clinical sign of metastatic gastric carcinoma. J Dtsch Dermatol Ges. 7:893–895. 2009
Kim HJ, Min HG and Lee ES: Alopecia neoplastica in a patient with gastric carcinoma. Br J Dermatol. 141:1122–1124. 1999.
Lifshitz OH, Berlin JM, Taylor JS and Bergfeld WF: Metastatic gastric adenocarcinoma presenting as an enlarging plaque on the scalp. Cutis. 76:194–196. 2005
Lookingbill D.P., N. Spangler, F.M. SextonSkin involvement as the presenting sign of internal carcinoma. A retrospective study of 7316 cancer patients. J. Am. Acad. Dermatol., 22 (1) (1990), pp. 19-26
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.