Blood test and Hair Loss: Necessary but Often Normal
Blood tests in Patients with Hair Loss
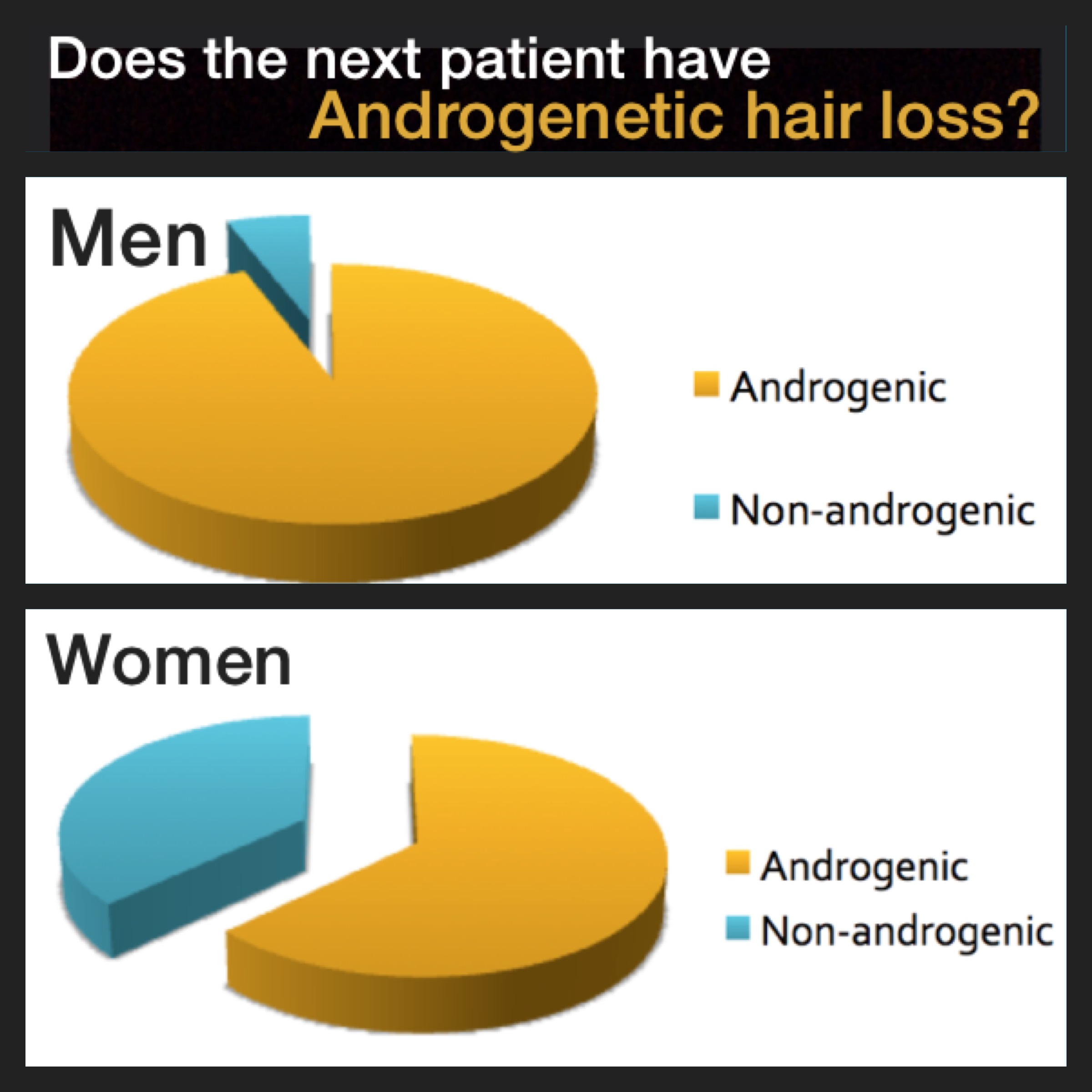
Hair loss for most is due to changes happening within the tiny hair follicles deep under the scalp. There may be a difference in the expression of certain genes or their may be different levels of inflammation surrounding hairs. It comes as a surprise to many patients that blood tests are often normal.
Why do we need blood tests if they are likely to be normal?
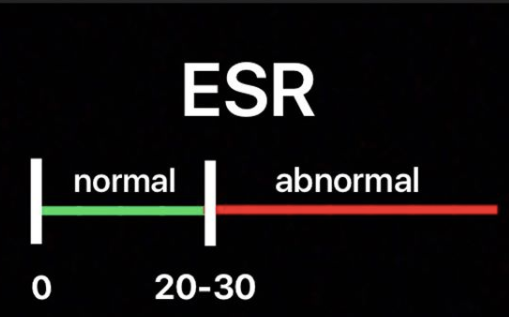
We require blood tests because there are many mimickers of hair loss and many conditions associated with abnormal blood tests are asymptomatic. If we could tell with 100% certainty that a given patient had low iron or had a thyroid problem just by listening to their story or examining their scalp, we would not need blood tests. The reality is that we can't. Many systemic conditions that can contribute to hair loss are asymptomatic. Low iron, thyroid abnormalities, zinc abnormalities, autoimmune markers, hormonal changes - these can frequently be asymptomatic.
Does it make sense that blood tests can be normal and still have hair loss?
It makes a lot of sense when one pauses and reflects on what is happening for most people. As mentioned earlier, hair loss for most patients is due to changes happening within the tiny hair follicles deep under the scalp. There may be a difference in the expression of certain genes or their may be different levels of inflammation surrounding hairs. The key tests that we need are therefore 'hair tests' not blood tests. In the present day and age, we don't have very sophisticated "hair tests."
I often use several analogies with my patients. If your arm was hurting and your doctor sent you for a chest x-ray, you wouldn't be surprised if your chest x-ray results came back normal. it is certainly possible that something in the chest is causing arm pain, but not very likely for most. What you need are tests on the arm - not tests of the chest. If you have chronic headaches and your physician sends you for an MRI of the foot, you won't be surprised if the MRI results of the foot come back normal. Blood tests may also be important in patients with chronic headaches - and sometimes these blood tests do reveal a cause of the headaches. But more often than not what is needed is tests specifically targeting to the brain - such as an MRI, CT or other related tests.
Conclusion
Every patient with hair loss needs blood tests to rule out a range of conditions that can cause hair loss and be asymptomatic. The typical blood tests that I recommend as a starting option are found in the following link.
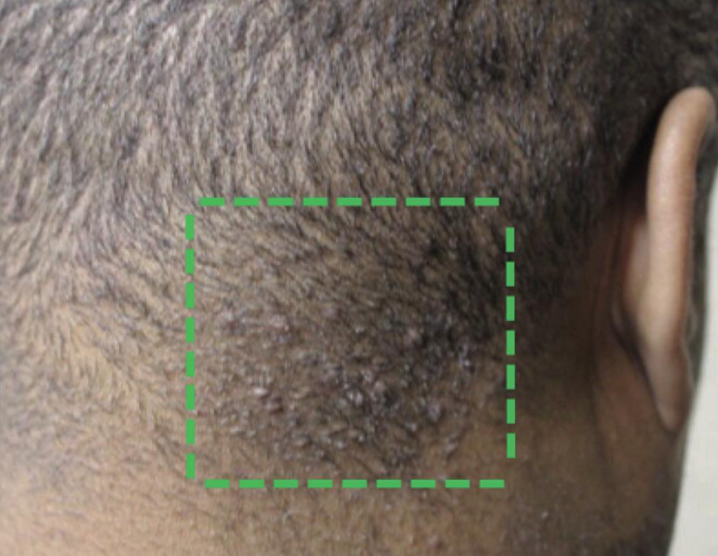
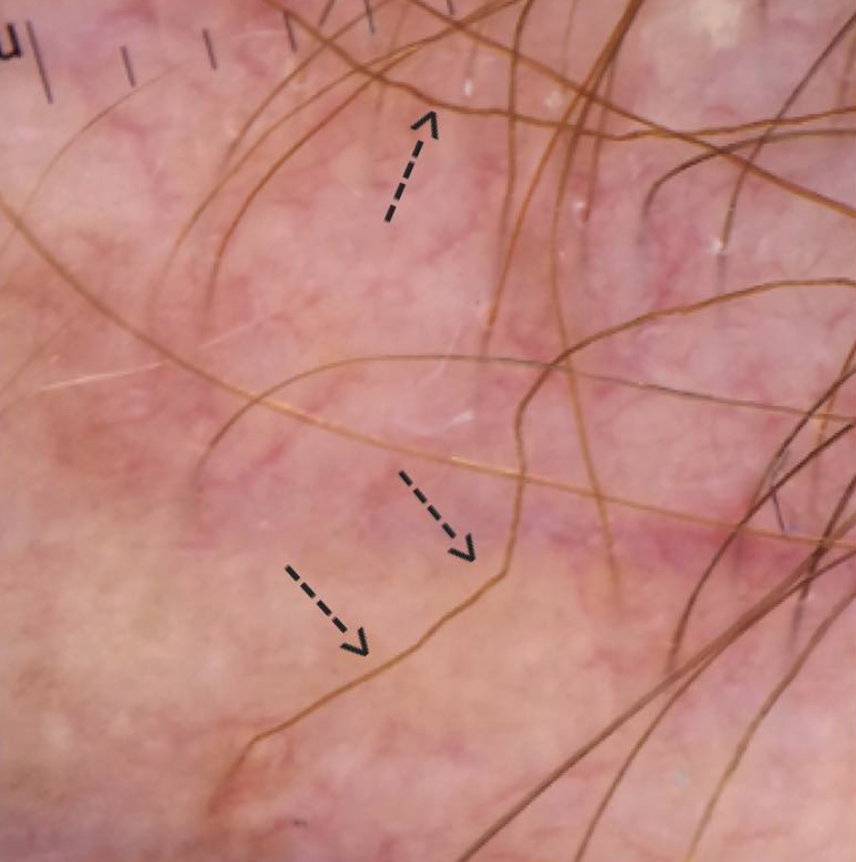
One should always be prepared for the possibility (and likelihood that blood tests will come back normal for many patients. We have only a limited number of "hair tests" in the present day. These include punch biopsies, clinical examinations, trichoscopy, pull tests, pluck tests, hair collections. and hair mineral analyses (which are not useful for most), and hair toxicology screens (which are not relevant for most). We do not have an ability to easily tests the thousands and thousand of different genes expressed deep down inside the hair follicle and therefore rely on the above ancillary tests to get a sense of what might be happening inside of a tiny hair follicle.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.