Scalp Biopsies For LPP: Wonderful Tool When Used Properly
Scalp biopsies are wonderful tools but they must be interpreted properly. Getting a scalp biopsy “just because” it sounds like a good idea is rarely every never a good idea. One needs to have a purpose of doing a biopsy - to rule in a disease or rule out a disease.
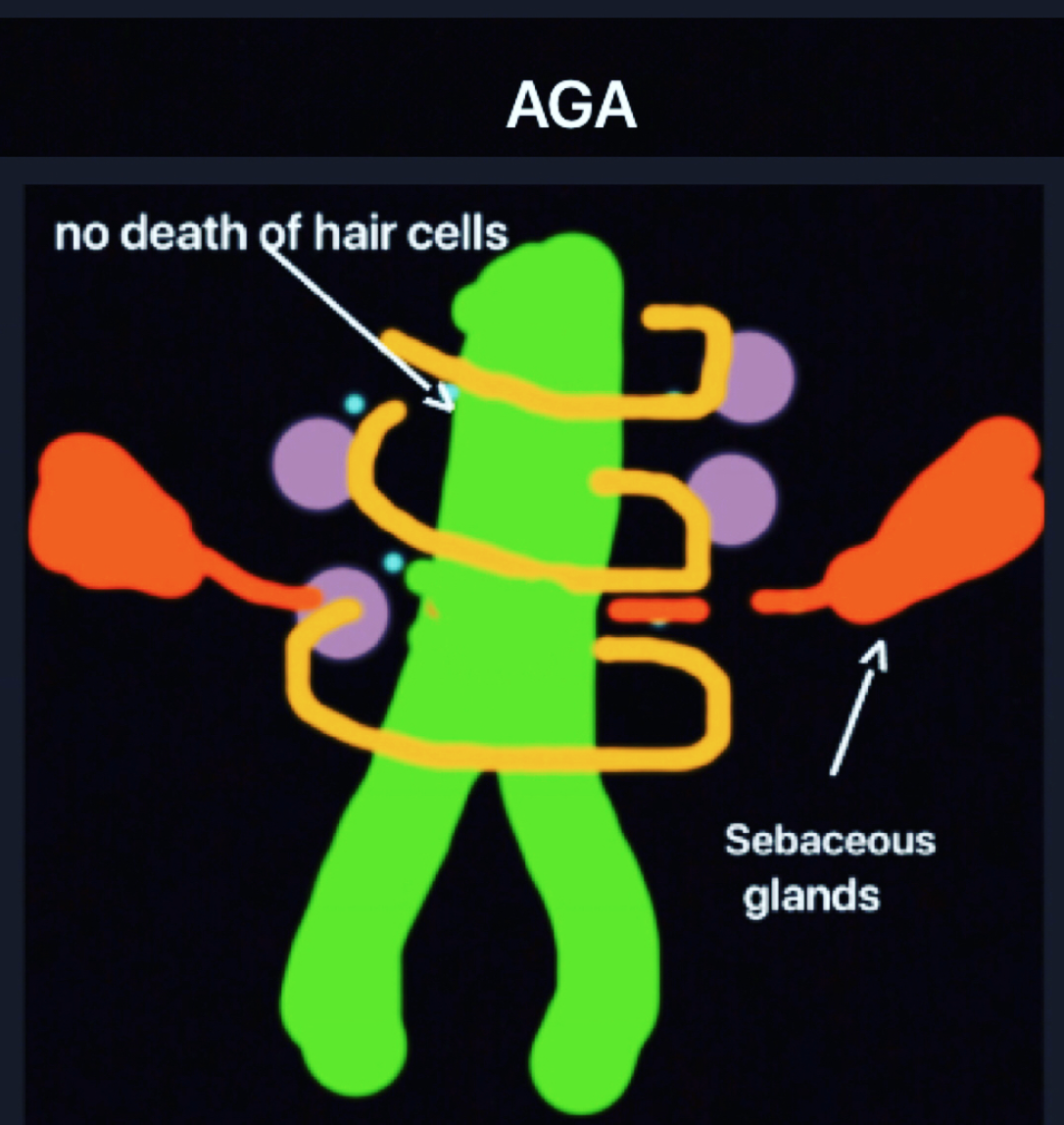
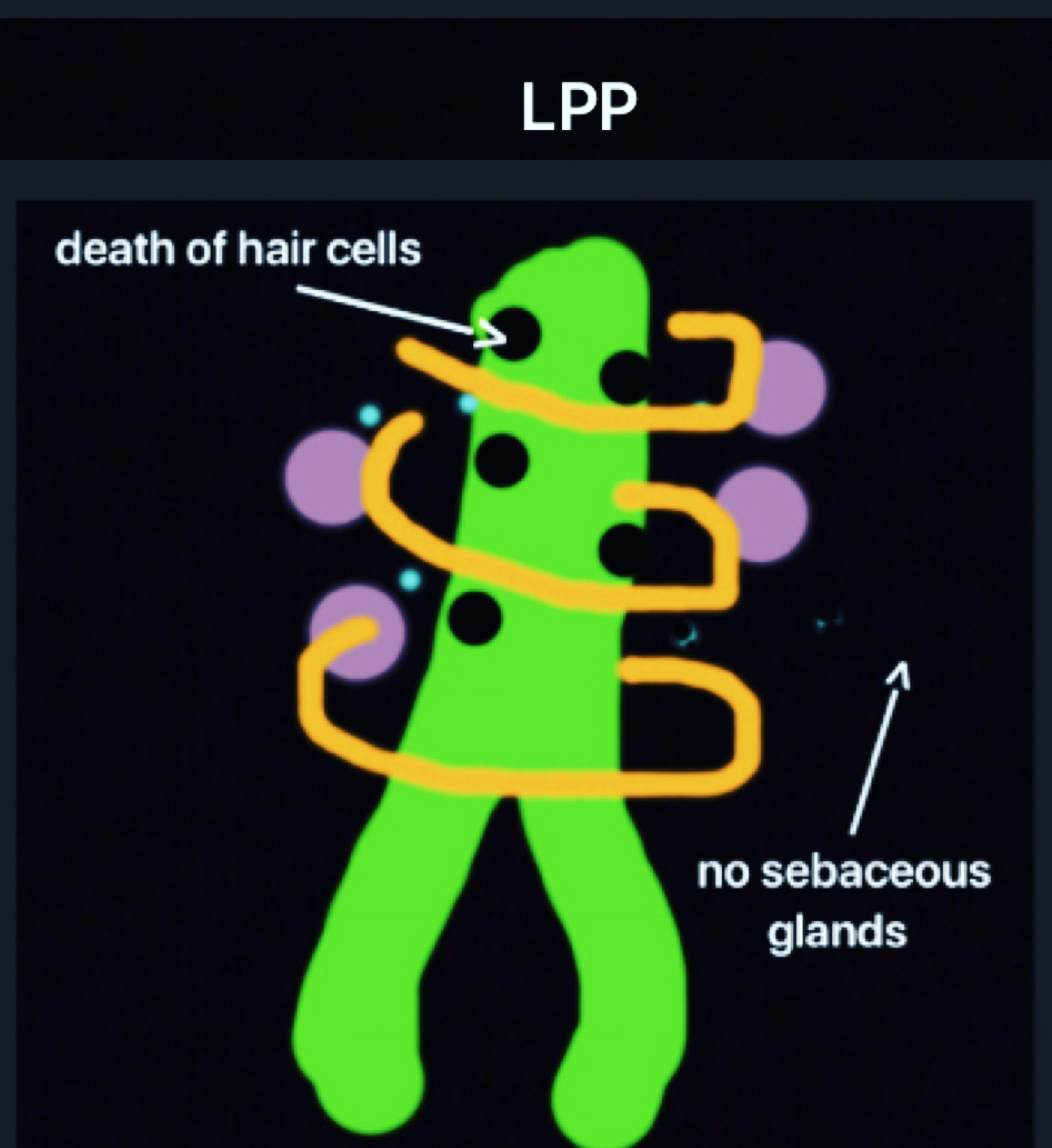
There is much confusion when it comes to diagnosing LPP and AGA. Every year I see at least 30 patients who come into through my office with a diagnosis of LPP and leave my office with a diagnosis of AGA. It's not some treatment I did that changed the diagnosis, it's the diagnosis that changed. It’s a pretty remarkable and sometimes emotional consult.
How’s this even possible? How can a diagnosis be wrong?
First off, let me say that most people who come into the office with a diagnosis of LPP actually have LPP. So what we are talking about here is something specific.
There is, however, tendency to overcall or overdiagnose LPP on account of a failure to recognize a few points. First, perifollicular inflammation and fibrosis is common in AGA. In fact, nearly 75 % of patients with AGA have perifollicular fibrosis and 30-40 % have perifollicular inflammation. So these alone are certainly not criteria for LPP! What needs to be properly recognized is that LPP is associated with “lichenoid change” in the outer root sheath and death of hair follicles keratinocytes.
The other cardinal feature of scarring alopecia is loss of the sebaceous glands. These latter two features need to be the focus of the pathologist’s attention and not solely the perifollicular fibrosis and inflammation. As simple as it sounds, many lives can be altered be understanding these principles.
REFERENCES
Evaluation of Perifollicular Inflammation of Donor Area during Hair Transplantation in Androgenetic Alopecia and its Comparison with Controls.
Nirmal B, et al. Int J Trichology. 2013.
Diagnostic and predictive value of horizontal sections of scalp biopsy specimens in male pattern androgenetic alopecia.
Whiting DA. J Am Acad Dermatol. 1993.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.