Pumpkin Seeds and Oil: What is the latest research?
What is the latest research?
There’s little doubt that pumpkin seeds and pumpkin seed oil are good for most humans in modest amounts. However, there is still some debate as to whether pumpkin seeds and pumpkin seed oil (PSO) are beneficial for hair loss and how much exactly one should consume.
A good deal of excitement surfaced in 2014 when a study by Cho and colleagues showed that 40 % of men using 400 mg per day of pumpkin seed oil had measureable improvements in their “male balding” (androgenetic alopecia) compared to men in the same study using just placebo.
Surprisingly, good studies of pumpkin seed oil for treating hair loss have not been replicated nor published since that 2014 study first came out and so we are left with some uncertainty as to the true benefits of pumpkin seed oil.
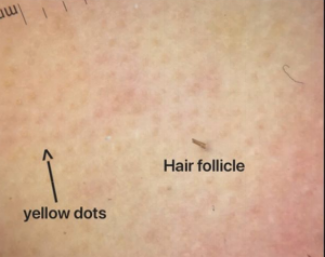
I continue to follow the medical research in the field. I’m interested not only in potential benefits for male balding but the potential for pumpkin seeds to affect the fats and lipids in the skin and of course the hair follicle. Many hair loss conditions, especially scarring alopecias, arise from altered “pro-inflammatory” lipids in the hair follicle. It’s clear that some dietary sources have a remarkable ability to change aspects of our physiology.
Pumpkin seeds are extremely rich in antioxidants and minerals. There is some evidence that they possess 5 alpha reductase abilities and so could impact conditions affected by androgens. Male balding, of course is the prototypical hair loss condition affected by androgens.
But pumpkin seed oil may have other anti-inflammatory properties. They may alter a variety of lipids but studies are limited to date. A recent study in rats showed that pumpkin seed oil at 100 mg/kg affected a variety of lipid metabolic enzymes such as fatty-acid synthase, acetyl CoA carboxylase, carnitine palmitoyl transferase-1, HMG CoA reductase. Pumpkin seed oil also reduced inflammatory markers such as TNF-α and IL-6.
Four years after the Cho research study, I don’t think we’re all that much further ahead in understanding the exact role of pumpkin seed oil when it comes to hair disorders. More research is needed.
Reference
A K et al. Arch Physiol Biochem. 2018.
This article was written by Dr. Jeff Donovan, a Canadian and US board certified dermatologist specializing exclusively in hair loss.